General Discussion
Related: Editorials & Other Articles, Issue Forums, Alliance Forums, Region ForumsThis message was self-deleted by its author
This message was self-deleted by its author (WilliamPitt) on Fri Apr 4, 2014, 02:41 PM. When the original post in a discussion thread is self-deleted, the entire discussion thread is automatically locked so new replies cannot be posted.
truebrit71
(20,805 posts)....you nailed it the first time 'round...
WilliamPitt
(58,179 posts)I helped, in my own small way, to promote this thing, because of the pre-existing conditions aspect that would benefit my wife. I feel like a fucking dupe.
On edit: I AM a fucking dupe. Last time that happens.
![]()
truebrit71
(20,805 posts)...and I was in the same boat regarding the pre-existing condition thing...not encouraging to hear that it too was a bait-and-switch...
wordpix
(18,652 posts)So far my med. bills have been astronomical for specialists, diagnostics and major surgery, but most have been paid by insurance. Without ACA my pre-existing condition would make me ineligible for any insurance, and right now I'd be broke and would be looking at selling my condo---this after a lifetime of work and nearing retirement age.
So I thank Pres. Obama from the bottom of my heart. Just remember he tried to do more but was blocked and compromised by the repukes, who are still trying to end O-care. Direct your anger where it needs to go---against the repugs
truebrit71
(20,805 posts)...but I will be angry at whomever deserves it...
wordpix
(18,652 posts)I was having probs with my private insurance co. that said I'd be cut off from finishing my contract before the ACA became operational. I also had probs with the ACA website in my state, making calls on way-too-busy phone lines, etc, and I contacted my Congressman's office. They gave me a health care constituent services rep, who was invaluable in dealing with my complaints. I had her email address and phone no., and we were in regular contact as each problem cropped up until the resolution.
Jefferson23
(30,099 posts)All the best to you with your recovery.
Dorian Gray
(13,786 posts)but it sucks that we have to do this and advocate so hard.
I truly wish the ACA went further. In the deepest recesses of my heart, I pray that this moves toward Single Payer someday.
Mojorabbit
(16,020 posts)I have had some help from grants but that is running out so I will have to go off the med again. I don't know who can afford that kind of copay. You would have to be a multimillionaire to do a lifetime of this medicine. I hope you can find some help so that she can resume her treatment. ![]()
TrollBuster9090
(6,053 posts)A) For which medication? (Is it an experimental drug? As I understand it, there is no effective treatment for MS, just standard drugs (like corticosteroids) that manage the symptoms and episodes; while some of the experimental ones like Amantidine haven't been proven effective, and therefore are not covered.)
B) I thought Medicare Part D was now obsolete, and
C) That's a copay of $20,000 per year. I thought the ACA limited copays to $5000 per year, unless Medicare isn't included, or you're talking pre-ACA?)
Mojorabbit
(16,020 posts)and I am paying for it at this time. It is Medicare with the part d plan from United. It is a pill which is glorious after doing the injections for so long. I still do the steroids etc to manage symptoms.
steve2470
(37,468 posts)It's damn expensive at retail prices, $4,868.41 a month. Good thing you can get it !
truedelphi
(32,324 posts)But now the $ 1,600 a month means she cannot.
Pharaoh
(8,209 posts)This is the question that is never asked by anyone. Why is that?
Most of the chemicals in drugs are super cheap. But they can charge what they like as some people need these drugs just to function, or to just stay alive. Yay capitalism and for making a profit on your life/death.......
steve2470
(37,468 posts)Hoyt
(54,770 posts)There's a lot of research, failures, expensive FDA approval, big lawsuits when an adverse effect occurs, etc.
While I would have no problem with all drug research, production, etc., being done by the government, they would likely not pursue a lot of these type of drugs.
Pharaoh
(8,209 posts)viagra was discovered by mistake, researching a blood pressure drug. Viagra = $18.00 per pill.
I don't know but do the math. The chemo drugs are astronomical.......why? Because people are told they will die with out them. Not necessarily true either BTW.
But, agree to disagree. Don't want a long argument thread! ![]()
Hoyt
(54,770 posts)Pharaoh
(8,209 posts)Pharaoh
(8,209 posts)Hoyt
(54,770 posts)let the government do it and pray the white wing Republicans keep funding drug programs, like they back all other social programs.
Doctor_J
(36,392 posts)Krugman called it the middleman multiplication act.
Hoyt
(54,770 posts)wordpix
(18,652 posts)Lots more on the web.
I'm a cancer patient and can't get it legally in my state yet, even though med mj is legalized for 2 years. Cannabidiol has antitumor properties. I am lobbying in my state now to get moving on mm and get the dispensaries up and going.
Mnpaul
(3,655 posts)when Billy Tauzin was welcomed with open arms at the WH while the single payer folks were told to take a hike.
Doctor_J
(36,392 posts)He forced the president to give big insurance 600 billion dollars a year
pnwmom
(109,801 posts)So does Canada's. So does Medicare and Medicaid's.
This has nothing to do with the ACA, except that his broker gave him false information about his choices. The ACA requires all insurance companies, on or off the exchange, to accept all patients, including those with preexisting conditions. Each insurer has its own formulary, so he should be comparing all the plans offered in his state to see if any of them list the particular drug his wife needs.
truebrit71
(20,805 posts)Very simple.
pnwmom
(109,801 posts)The British National Formulary (BNF)[1][2][3][4][5][6] is a pharmaceutical reference book that contains a wide spectrum of information and advice on prescribing and pharmacology, along with specific facts and details about many medicines available on the National Health Service (NHS), including indication(s), contraindications, side effects, doses, legal classification, names and prices of available proprietary and generic formulations, and any other notable points.[7] Though it is a national formulary, it nevertheless also includes entries for some medicines which are not available under the NHS and must be prescribed and/or bought privately (such as alprazolam tablets or minoxidil solution). A symbol clearly denotes such drugs in their entry.
truebrit71
(20,805 posts)When they need meds, they get meds. No hoops to jump through...Doctor prescribes them, they take them. No muss, no fuss.
Of course the conservative arseholes in power are trying to destroy the NHS anyway they can, so I'm sure there will be "market-based improvements" brought to bear...but hopefully they will be removed from power next year...
pnwmom
(109,801 posts)The same as doctors here do with Medicare patients, whose choices are also limited by a formulary.
http://en.wikipedia.org/wiki/Formulary_(pharmacy)
United Kingdom[edit]
In the UK, the National Health Service (NHS) provides publicly funded universal health care, financed by national health insurance. Here, formularies exist to specify which drugs are available on the NHS. The two main reference sources providing this information are the British National Formulary (BNF) and the Drug Tariff. There is a section in the Drug Tariff, known unofficially as the “Blacklist”, detailing medicines which are not to be prescribed under the NHS and must be paid for privately by the patient.
In addition to this, local NHS Trusts, including Hospital Trusts and Primary Care Trusts (PCTs), produce their own lists of medicines deemed preferable for prescribing within their locality or organisation; such lists are usually a subset of the more comprehensive BNF. These formularies are not absolutely binding, and physicians may prescribe a non-formulary medicine if they consider it necessary and justifiable. Often, these local formularies are shared between a PCT and hospitals within that PCT's jurisdiction, in order to facilitate the procedure of transferring a patient from primary care to secondary care, thus causing fewer “interfacing” issues in the process.
As in the United States, NHS trusts actively encourage generic prescribing, in order to save more of the budget allocated to them by their Strategic Health Authority, and ultimately, the Department of Health.
OwnedByCats
(805 posts)The NHS runs perfectly compared to these insurance companies that make everything complicated, all in aid to screw you.
HuckleB
(35,773 posts)Spider Jerusalem
(21,786 posts)CaliforniaPeggy
(153,358 posts)K&R for this most excellent rant.
![]()
uppityperson
(115,920 posts)I do hope that is not what you meant.
CaliforniaPeggy
(153,358 posts)I'm just agreeing with Will.
uppityperson
(115,920 posts)Without that, no problem
CaliforniaPeggy
(153,358 posts)uppityperson
(115,920 posts)on Pres Obama as it is not all hos. Blame congress, ins companies, and even Will for not checking to see if it was covered. It sucks, but to rant at Obama that way? bah
Best wishes to all with their healthcare, and insuruance companies are legalized gambling out to make a profit.
JEB
(4,748 posts)Death and agony are their stock in trade. Fuck'em all.
magical thyme
(14,881 posts)it's Anthem or nothing, iirc.
truedelphi
(32,324 posts)Mid August the summer of 2009.
Stewart: So a university student at U of Colorado Boulder, asks the President about public option, and the student seems to have the idea that public option is related to socialism or being a commie.
Does Obama take a moment to educate the young man. No instead, he apologizes for the existence of public option by saying (I am paraphrasing) 'Public option is but one tool in an entire tool box of options that Congress can employ. But since I am the President, and I am part of the Executive Branch of the US government, the separation of the three branches of government means I must bow out of the discussion until Congress has put its finishing touches on the piece of legislation that they re putting together.'
#### End of Stewart related material
Then we all come to find that while Obama is claiming his lack of using the bully pulpit for the public option, his own Chief of Staff, one Rahm Emanuel, was meeting with Liz Fowler to put together everything that the Big CEO types from, Big Pharma and Big Insurance wanted.
What is going on right now inside America's Body Politic is that people have had it. Over the last week, I have been tabling on an local issue, unrelated to party politics, and what I am hearing again and again is "Sorry but I quit voting."
Most people will just give a grin and giggle and say, "you know," when I ask why they won't vote in June.
But some people articulated that they see no real reason to vote in a rigged system. One man spent some ten minutes tracing his life as a voter, concluding with, "Well in 2012 they told me they were the lesser of Two Evils, and I kept hearing a voice in my head say, 'Lesser of two evils is still evil.'"
I concur with that man. If there is no one in Washington or in a leadership position in either party that cares about reforming politics, outside of maybe Bernie Sanders, or Liz Warren, with the rest of them being whores to Big Corporations, then why should I give a rat's ass in hell about the Democratic party?
uppityperson
(115,920 posts)Edited to remove un needed snark with apologies.
truedelphi
(32,324 posts)So don't put them in my mouth.
But I did say that this whole situation of having two parties bought and paid for by Big money is pathetic.
And it is also as one other poster pointed out here, Fascism.
That "F" word is a far greater indictment than the swear words. You can be offended that angry people are using "anger words," or you can be offended that we have devolved as a meaningful republic with free elections, and are now ruled by whores to Big Business, it is your choice. I know what I am offended by.
uppityperson
(115,920 posts)but cursing out the president and calling him a used car salesman doe snot address the issues. And isn't needed on DU to discuss wtf is going on and wtf to do about it.
Again, my apologies.
hfojvt
(37,573 posts)is still greater.
The conservatives in this country, the Koch billionaires are still out there electing Republicans and pulling the Republican party always to the right, to the right, to the right.
I am sure they will be happy if we stop resisting that.
Enthusiast
(50,983 posts)When the President took office he had a MASSIVE mandate.
Instead the President said that single payer was a bridge too far and would be "too expensive". Well, he knew better. He knew damned well that single payer would have been substantially cheaper but it would lock out the for-profit vulture killers.
President Obama deserves considerable blame.
red dog 1
(30,567 posts)President Obama should have at least TRIED to get a single-payer health plan; but he didn't.
As far as the OP:
I agree with : "Fuck you, insurance industry"
But I don't agree with:"Fuck you, Mr President, you piece of shit used-car salesman."
I posted an OP on the possibility of changing the ACA into either single payer or a universal health care plan
"Can Obamacare be changed to make it a single payer health plan?"
http://www.democraticunderground.com/10024670957/
Enthusiast
(50,983 posts)Somehow, the ACA allows individual states to enact a single payer system as Vermont has. I believe California is trending that way also.
We must have single payer now! There are far to many of us suffering because of the greed factor.
Scuba
(53,475 posts)kelliekat44
(7,759 posts)the insurance and pharma-industrial-complex in my opinion. It is all so much bigger than one President. I believe an appeal is in order, first , and than a reasonable complaint to the President conveying what you have learned that I am certain he has no idea that this is happening We are in the first stages of trying to make the ACA really work for us all. It seems a bit unfair that the criticism should be so unforgiving at this point. What is this really about?
uppityperson
(115,920 posts)brush
(59,431 posts)He ranted about the President using the injured Sargent Cory Remsburg as a prop during the State of the Union speech.
He totally missed the point that the President was trying to make — that the kind of injuries the solder suffered were the results of endless wars with endless deployments. The President called for the end of our constant war footing.
It was the first time in my lifetime that a sitting president made an anti-war remark.
It was extraordinary but, somehow it was too subtle for Pitt and he posted an even worse rant against Obama. Makes you wonder about people who fly off the handle with mis-targeted anger — especially the ones with supposed gravitas.
Cha
(309,260 posts)easy to do because he was down there working on the worst angle he could possibly come up with.
JI7
(91,658 posts)brush
(59,431 posts)quakerboy
(14,319 posts)Maybe he doesn't even have a wife. Or if he does, he probably doesn't even really care about whether she has access to medication that she needs. Because he's just playing at being a living, caring person with a family. ![]()
Its amazing to see the heartlessness here, from people claiming to be democrats or progressives. Care about our fellow man? Not if it might impede our ability to praise the political figure of our choosing!
Jakes Progress
(11,209 posts)if he just wrapped himself up in Obama-Glo and ignored his wife's pain. Blind adoration is a great salve.
Cha
(309,260 posts)more cognizant rant if he were actually throwing his ugly insults at whomever was actually causing the problems with his wife's meds.
How true. Because the millions of people who can now get insurance don't matter because his wife's medicine isn't covered.
blame express scripts, blame optum RX, blame United healthcare, blame anthem, blame big Pharma, blame Lieberman (fuck him), blame Bayh. Blame everybody.
But the president did what he could to get as many people insurance as he could. Is it perfect? No. Is it a good start? Yes.
Go fight for the coverage. There's lots of good advice in this thread that tells you what to do. Start with the insurance company, go to the Department of Insurance, find a lawyer friend who can help write letters. But fuck the president because you didn't get coverage for a drug? Nope.
Response to sobenji (Reply #525)
Post removed
truebrit71
(20,805 posts)Sick of the compassion-free, toe-the-liners around here..
kath
(10,565 posts)Too bad it was hidden.
truebrit71
(20,805 posts)..![]()
And boy there's a lot of them around it seems...
quakerboy
(14,319 posts)after reading the first few responses, a fairly equivalent but less well spoken rant was in my mind. Everyone should take the time to unhide this. And the fact a jury hid it, over all the other crap ive seen fly by unhidden, says some ugly things about DU.
And a hearty fuck you to every person posting like a heartless Republican on this thread. Democrats have compassion. You do not. You have outed yourself to anyone who is paying any attention, though you will likely skate by for now because you are pretending to be aligned with Democrats.
truebrit71
(20,805 posts)...especially looking at some other posts that were left alone...although it was fairly obvious by some of the responses that the apologists are well-coordinated..
Cha
(309,260 posts)was a nasty piece of ignorant work.
Auntie Bush
(17,528 posts)Autumn
(47,627 posts)There are ten different health insurance companies in NH. According to the independent (family friend, ally) insurance adjuster I spoke to at length this afternoon, pursuing coverage with any of them would be a waste of time. Why? Because - according to dude - the whole "You cannot deny coverage to people with pre-existing conditions" thing only applies to insurance companies within the ACA network. You heard all that shit about "Grandfathering." Well, this is that, and all of them will turn us down because they still can.
I am in the process of running down the facts of the matter, but family friend and ally was confident enough to basically tell us not to bother.
So yeah, that, too.
Autumn
(47,627 posts)I'm so sorry Will.
Nye Bevan
(25,406 posts)Any insurer selling individual health plans (whether on or off the exchange) in your county cannot discriminate based upon pre-existing conditions. (However, grandfathered plans that are not being sold anymore will not be offered to anyone, whether or not they are in good health). Here in CT we have an off-exchange policy which I bought because all of the exchange policies offered only very narrow networks which excluded most of our doctors. Approval was immediate and without any questions about health. (The off-exchange policies are not eligible for subsidies but are still guaranteed issue).
For example, if you go to Anthem.com and enter your zip code to browse individual health insurance policies, you will get check boxes to choose between "Marketplace" and "off-Marketplace" plans. The "off-Marketplace" plans are not in the ACA network but are still guaranteed issue.
As far as the drugs go, yes, this is frustrating, but you need to persevere. Have every doctor you can write a letter explaining why this drug is essential. Make copies of previous prescriptions to show that your wife has been using this drug for a long time. And send all of this documentation with a polite but insistent appeal that this drug be covered. If the appeal is turned down, immediately appeal to the next level. If you have already reached the top level, immediately file a complaint with your state's health insurance department. I have needed to do this a few times over the years here in CT and not once have I ever failed to eventually get coverage of whatever I wanted. The impression I get is that their business model is to routinely deny coverage secure in the knowledge that many people will just give up, but the persistent complainers who keep escalating their complaints eventually get what they want. In particular, going to the state insurance department always seems to suddenly make them take you much more seriously.
QuestForSense
(653 posts)You can't even pay people to give you advice that is half this good.
crim son
(27,530 posts)none of it should be necessary.
Whisp
(24,096 posts)that ain't gonna happen.
Lex
(34,108 posts)so it has worked
Whisp
(24,096 posts)Lex
(34,108 posts)Persistence is key. And being the squeaky wheel.
ConservativeDemocrat
(2,720 posts)Hopefully William Pitt will realize that for once.
- C.D. Proud Member of the Reality Based Community
Lex
(34,108 posts)about people not being able to get their preferred drug for a chronic health issue.
Whisp
(24,096 posts)because of what they claim he did to them.
There is a post here somewhere with an animated pic of Obama laughing (apprently at the OPs problems).
now that is a piece of shit thing to say.
ohheckyeah
(9,314 posts)the preferred drug for a chronic health issue is marijuana.
Jesus Malverde
(10,274 posts)magical thyme
(14,881 posts)as well as emotional support and a load off his chest.
All of which are good things.
ConservativeDemocrat
(2,720 posts)Especially about formularies, which all medical systems have, even the vaunted single-payer.
- C.D. Proud Member of the Reality Based Community
magical thyme
(14,881 posts)however, I'm willing to cut people slack in the first wave of combined panic and anger when they discover something really, really bad regarding somebody really, really important to them. And when you're a writer by profession, then the screaming comes out in writing. ![]()
Certainly I refrain from blaming them or calling them foolish for making a poor choice, when choices were made under tight time constraints and were set up by the sales people to be as inscrutable as possible.
The formularies, as mentioned in several posts above, are not necessarily available for review until *after* you sign up, which makes it impossible to choose your insurer based on the formulary.
Other insurance industry "fine print" problems are surfacing, and will continue to surface. For example, I just posted about a problem with access to cancer centers. If anybody bothers to read the linked article (and of course many won't, they'll just shoot from the hip) it looks like the issue is going to be examined (and hopefully addressed) next year.
Doctor_J
(36,392 posts)do what they are supposed to do. Do you comprehend how moronic that is?
Whisp
(24,096 posts)the poster took the word of some 'personal friend' schmuck that there is nothing else to be done.
A lot of information, just in this thread, that says there is a Lot to be learned and done. He should do the damn homework instead of having another ridiculous tantrum. Tantrums will not do anything for the situation.
woo me with science
(32,139 posts)What this thread screams for us, yet again, is the actual level of compassion of the corporate Third Way - its utter contempt for the people it pretends to want to represent.
Corporate rule, whether Republican or Democratic, is all about the bottom line. It is about slick marketing of policies that profit the One Percent, rather than actually seeking to serve the needs of human beings. Corporatism is, by definition, about profit and *never* about human beings. No matter how many pretty promises we hear from corporatists during election years, the contempt you see in this thread is the actual level of compassion that will be offered when actual human beings are harmed by corporate policy.
ctsnowman
(1,903 posts)is the right word.
ohheckyeah
(9,314 posts)because you aren't a good little citizen/consumer. ![]()
NCTraveler
(30,481 posts)They are doing what they are suppose to be doing. Making profits. And they were just given a gift. Not debating you as I pretty much agree with you, just wanted to add what their main goal is. Profits. Their job is to care for investors, not provide healthcare.
Doctor_J
(36,392 posts)and as I sat listening to her tell us all of the wonderful features of company's offering (my annual deductibles this year went from $500 to $8300), that thought kept rolling through my mind. Her job is selling insurance and making money for herself and her CEO. It has nothing to do with keeping me healthy.
NCTraveler
(30,481 posts)Truly sorry about your deductible. You are absolutely correct. She was there to sell you health insurance, not health care.
sabrina 1
(62,325 posts)have to work so hard to stay alive in this country. While Will can probably do all this, there are untold numbers of people who do not even know how to use a computer, or have anyone to help them wade through all this. And to have to PAY to be so abused, is unconscionable.
Health Care should be a right, but here people are just commodities and the rights go to Big Pharma and the Private Insurance Corps who mostly wrote this legislation. Their right to profit, trumps OUR right to live. It's better that people understand how it is, rather than remain hopeful that there is someone within this system who actually cares about them.
Wendell Potter, Whistle Blower described it perfectly when he told how shocked he was to see Americans lining up for a Third World charity organization, then operating here, in the US. Of seeing Americans being treated in Animal Stalls, desperate for care they could not afford. It touched him enough to go back to his HC Corp and show them his photos, hoping to get a reaction similar to his own very human reaction.
Instead, when he asked them what they saw, what they thought of it the response was 'More Customers'. But how, they had no money which is why they were there?
Now we know. Privatize Medicaid, force everyone to buy HC, if the can't afford it, the Health Ins Corps get it from Medicaid instead of that money going directly to the hospitals and doctors.
As that Public Fund, passes through their greedy hands, 20% or more is pocked by them.
What a scheme, if only we all could pull off something like this.
Nye Bevan
(25,406 posts)but I entirely agree that it is a monstrosity that people should be forced to jump through these hoops to get treatment for diseases. Health care is not a commodity that should be managed by the pursuit of profits.
sabrina 1
(62,325 posts)never have allowed to be 'for profit'. There was just too much room for abuse. Or at least there should have been an option for National HC.
questionseverything
(10,654 posts)it will do no good to complain to state ins board if his contract denies it
(and you know that)
Nye Bevan
(25,406 posts)On two of these occasions when I used the insurer's appeal process the decision was reversed. On the other occasion the decision (not to cover) was upheld but then when I complained to the state insurance department they agreed to cover it.
steve2470
(37,468 posts)A company will only refuse you if it really screws them over long-term and/or hurts their public image. Health insurance management looks awfully cold-hearted denying needed meds for people, especially children, the disabled or the elderly.
questionseverything
(10,654 posts)now if you were arguing over what is "reasonable and customary" then yes there is contract language that state ins department could help with
but if you are saying you got something covered that was not in contract......I call bs
without knowing what will has in his contract's language, it is impossible to tell
Nye Bevan
(25,406 posts)with this kind of language:
Non-formulary exception process
The non-formulary exception process provides physicians and members with access to non-formulary drugs and facilitates prescription drug coverage of medically necessary, non-formulary drugs as determined by the prescribing practitioner.
Patients can also have a non-formulary drug without invoking the exception process anytime by paying full price for the drug if the prescribing provider deems the non-formulary drug not medically necessary, but agrees to prescribe the drug due to patient demand.
The prescribing practitioner makes the final decision regarding what drug is appropriate for the member. Non-formulary drugs should be used only if the patient fails to respond to formulary drug therapy, has an adverse reaction to formulary drug, or has other special circumstances requiring the use of a non-formulary drug.
questionseverything
(10,654 posts)as you described....and as I pointed out the ins would pay only if the proper language was in contract
we still do not know what will's contract says
maybe you would like to field this question of mine////////////////////
http://www.bcbsil.com/PDF/rx/rx_list_std_il.pdf
Specialty drugs
Specialty drugs are used in the treatment of medical conditions such as hepatitis, hemophilia, multiple sclerosis
and rheumatoid arthritis. Specialty drugs may be oral, topical or injectable medications that can either be
self-administered or administered by a health care professional. For a current list of specialty medications,
visit myprime.com or bcbsil.com and log in to Blue Access for Members.
Note that some drug classes may be excluded by some plans and therefore may not be covered under your
pharmacy benefit. Your plan may have a different coverage level for self-administered specialty drugs. If you
have questions about your coverage for specialty medications or your prescription drug benefit, call the
number on the back of your ID card.
////////////////////////////////////////////////////////
how do I look it up before I buy?
I have to be a member before I can see the list
cimzia is what I am looking for
/////////////////////////////////////////////
cimzia is about 1600 bucks a month retail so the 700/month cap would screw us over too
Nye Bevan
(25,406 posts)Which sucks and is frustrating. I looked up cimzia on my plan and all it told me was that pre-approval was required (it would not even give a price). For this drug, however, the manufacturer's website seems quite helpful (go to http://www.cimzia.com/cimplicity/patients.aspx). They have a copay savings program where they help you verify insurance coverage and you get a savings card which (they claim) resulted in no out-of-pocket costs for 97% of the participants in 2013. It sounds like what they do is help walk you through the approval process to help you get the drug approved and then absorb any deductible or copay themselves, just accepting whatever the insurance company pays them, with you getting the drug for no out-of-pocket cost. You should definitely look into this; I have used a similar manufacturer's program with another drug and the savings can be enormous. Good luck!
questionseverything
(10,654 posts)but that really is not the point being discussed here in this op is it?
will was told it was his fault for not knowing what is covered, I think you and I have just shown this is not necessarily true
so what it boils down to is even with insurance "we the people" are still going to be left to the mercy of insurance companies and big pharma.....this is what will's op clearly points to, emotions aside
Ms. Toad
(36,471 posts)or the doctor list prior to plan purchase. Those are two things I always check, because of long term relationships with doctors - and very costly meds.
Specialty drugs are relatively new - typically they are biologics. But they have nothing to do with the ACA. I'be been fighting that particular dragon for a around 5 years now.
questionseverything
(10,654 posts)but it gives no answers on specialty drugs....deliberately vague is probably the closest to the truth
and the reason it is related to aca is the aca did nothing to prevent the spiraling of med costs......cost containment should of been the first issue addressed
Ms. Toad
(36,471 posts)tobramycin inhal soln (Tobi – brand is NF)
INCIVEK
PEGASYS
ribavirin (Copegus, Rebetol – brands are NF)
VICTRELIS
FUZEON
- and many more in the rest of the list.
I don't see your particular specialty drug - so you should call them with the specific name of the plan you are considering and ask them if it is covered. It appears from they way they have the formulary set out that some specialty drugs are covered on all plans, and others are not uniformly covered - so you will have to ask about a drug which is not uniformly covered. If you are taking a specialty drug, it is probably worth it to make a phone call.
questionseverything
(10,654 posts)he had asked first thing if his wife's drug was covered,,,,,,ins says yes with a very simple procedure
that turned out to be untrue as she has been rejected twice
if you have fought as many successful appeals as you say you have you know, if it is not in the language of contract it is not covered
no verbal commitment matters
now in will's case I am sure his wife's needs will be met , he is fairly high profile but again I ask, what about those that are not high profile people?
what about those that do not have the time ,energy or means to fight big insurance?
and one more thing while I am at it........we do not know what will's spouses meds cost, some have suggested it is a new pill form of specialty drug that costs 4600 bucks a month....if that is true the economic model for aca is no way sustainable
some things are just too important to leave to a profit driven industry
Ms. Toad
(36,471 posts)But - before starting buying a new plan, I would have gotten the details in writing. It sounds like a step therapy drug - and from what he has said, it sounds to me like his doctor's office doesn't have a clue how to complete the proper forms.
The reason I say that is because one of the most medically competent doctors treating my spouse and daughter has zero clue about how to get approval for a step therapy drug. He started out by telling her that insurance probably wouldn't cover it - since he hadn't been successful in getting approval for anyone else. It is actually a very simple procedure - clearly described in the certificate of coverage (and explained to me over the phone). You have to get the doctor to certify that one of multiple other therapies have been tried, and are not suitable, and then it will be covered - because for most people there are better, cheaper, options which they want you to try first.
In our case, it took about a month, with the doctor repeatedly telling my spouse that they had appealed and been denied, and the insurance company repeatedly telling me they had no record of an appeal - and that it was a simple procedure to get step therapy approved.
What it came down to when I unwound it all was that the doctor was clueless, and my spouse did not give them the address/phone/fax for step therapy approval which I had told her to give them, because she assumed they should know how to handle insurance. They had been faxing a regular prescription to the regular prescription number, and having it rejected. They called the same division, who gave them other non-step alternatives, without mentioning that it was a step therapy drug. I was finally able to have the insurance company open a case for the step therapy. That allowed them to contact the doctor directly and request the documentation, and within a week we had the meds.
If it had been my doctor, it would have been straightened out in 2 days max - but this is one of very few doctors I "let" family members handle on their own, since (generally) he doesn't handle the family diseases where where someone with a mind adapted to handle medical matters is crucial (lots of rare/complex diseases in our family).
But making the insurance companies behave has nothing to do with being high profile. It does have to do with being persistent, with knowing your plan, and with having doctors who are either advocates by nature - or who are willing to advocate if you lead the way.
As far as the ACA being sustainable - the premiums are based on averaging the high cost of Will's wife's costs (and my daughter's costs) with the more typical costs that most of us have. They are sustainable - not ideal - but sustainable because that is how shared costs work (either insurance or single payer). I believe the average annual spend per person (including for those very expensive people) is around $5000. They would, of course, be both cheaper and even more sustainable if the insurance middleman was taken out of the picture.
questionseverything
(10,654 posts)I think this is one of those claims
you said,
I have won plenty of appeals for things which were not in the language of the contract./////////////////
so I would love to see the documentation
Aerows
(39,961 posts)live in either Canada or Australia, and thus don't have a fucking clue how screwed up health care is here. They are just defending Obama because he's Obama. They have absolutely no basis for comparison. If you ask them individually, they will admit it, but publicly, it's all Obama all of the time. Understand what you are dealing with - people that will tell you that the ACA rocks while they have never in their life gotten sick and then had to deal with hospital bills.
Ms. Toad
(36,471 posts)I'll give you enough details of a couple of examples sp that you can at least verify the condition and the difficulty of getting coverage at the time.
I have VTOS (upper extremity DVT), which dates to 1988. The first time I spent a month in the hospital because that was the only option for stabilizing on anticoagulation therapy before being discharged on warfarin. - normally the process of balancing the two anti-coagulation medications takes 5-7 days; my body was stubborn. The second flare, 1998, low molecular weight heparin (Lovenox) was developed - but was only approved for clot prevention in connection with surgery - not as a treatment for clotting disorders. The choice was spending several days in the hospital, or convincing the insurance company to cover outpatient use of Lovenox. With my doctor's assistance, they insurance companies were convinced to allow me the (then) experimental treatment.
Here's a 1999 article about the early reported use of it for outpatient treatment: Savage KJ, Wells PS, Schulz V, Goudie D, Morrow B, Cruickshank M, et al. "Out-patient use of low molecular weight heparin (dalteparin) for the treatment of deep vein thrombosis of the upper extremity." Thromb Haemost. 1999;82:1008–10. There was also an ER episode around the same time "ripped from the headlines' as another show likes to say, in which the more common outcome - denial of coverage - was the outcome. That study of 46 patients was published almost a year and a half after my insurance company was convinced to allow me to use it for that condition as an outpatient. And, a 1999 article which references 12/31/1998 FDA approval for marketing the use of enoxaparin for outpatient use for treatment of uncomplicated DVT - 7 months after my insurance company was convinced to pay for it.
Here is a link to a separate mention of my first rib resection which was done to treat the same problem more recently - next to last paragraph. I obviously must have planted it contemplating just this conversation. Feel free to confirm that first rib resection is the current favored treatment for VTOS.
Another minor victory in the same time frame - the pathology costs relating to removing a mole displaying pre-cancerous traits were covered, but the excision was denied. They routinely denied all mole removal "cosmetic surgery." I didn't have to get the doctors involved in that one - I just challenged them about whether they denied coverage for the surgical removal of breast tissue in to examine the tissue associated with apparently pre-cancerous changes as cosmetic breast reduction surgery. Kind of surprised they bought that one as easily as they did, but they did.
Finally, if you have had many encounters with surgery and insurance, you are aware (or if not you can easily verify) that anesthesiologists are entities unto themselves - and fairly frequently not covered by the same insurance policies as the hospitals in which they work. I had an emergency appendectomy, and the anesthesiologists were considered "out of network," even though the hospital was "in network." The closest "in network" anesthesiologists were more than 50 miles away - and all out of network care required advance approval. Despite not having advance approval, they ultimately granted my appeal because of the emergency nature of the surgery, combined with the lack of disclosure by the hospital that they were using an anesthesia team which was out of network. (Here's an article) which specifically mentions this issue with anesthesiologists
Just 3 of the more generic examples of the many appeals I have won. Sorry - I'm not posting documentation, but you should be able to at least verify that they are the kind of problems which routinely crop up with insurance that are either prohibited by the policy, or beyond the language of the policy.
questionseverything
(10,654 posts)i still do not think you won anything outside the scope of your language
the first example is closest since the drug you wanted was experimental but the treatment you and your doc wanted saved them a week plus of cost for in patient hospital charges
the second example, if pre cancerous was well with in your language to be covered
the anesthesiologists example rings a bell with me because I had to fight insurance companies for same except we had no network to bind us but ins denied it over and over, first saying it was included in surgeons bill, then saying that they had already paid for it (when actually they had just paid for the supplies), then they said the hospital billed them wrong..... so while I had insurance gal on cell phone I drove to the hospital went to billing clerk handed her phone after explaining to clerk the problem was her....she ripped that insurance gal a new one (in a very polite professional way) and when she got off phone it was covered
/////////////////////////////////////
our entire convo here is sad, what you are describing is how insurance deliberately denies what they rightly should pay (imagine how many people do not fight them and just pay it)
I am not sure why you are defending this system, I guess if you think it's good enough for you and yours you have a right to think that way....I do not agree
out of curiosity, with all your families medical issues how were you buying insurance before the aca? was it thru an employer?
because my house does not have anywhr near the medical problems you have described and we were priced out long ago
Ms. Toad
(36,471 posts)The first was not covered. It was not part of the formulary, nor part of the medical coverage. One of the articles I linked you to discussed how insurance companies dealt with it at the time (pretty much not at all). And - if you look for articles at the time, you will find it was routinely denied - even though it saved the insurance company a considerable amount of money. The stupidity of that is why it was popularized on at least one medical drama within a year of my experience with it.
The second was clearly, by the policy, excluded as cosmetic surgery. It was a ridiculous exclusion, but it was an exclusion.
As to the third - that is the closest to being covered in the language of the policy, in that there was an appeal process to petition to have out of network care treated as in-network. There's plenty more.
And, as I said, those are three which are either relatively generic and which I can point to historical or other outside references to provide some support (or, in the first instance, one I have mentioned on DU before).
As for coverage - it has been a variety of coverage over the years, made more difficult because I have a same gender spouse who has not been able to work for a decade (early onset Alzheimers).
We cannot buy insurance on the open market - prior to the ACA, it would have $15,000 - $20,000/year for my daughter alone, and far more for me based on age. Early in her life she was covered by Medicaid - during a period when my income was minimal and, because our marriage is not recognized, neither of us were eligible to be covered under my spouse's policy.
I had private insurance for a while, the company went out of business, and I discovered I was uninsurable by anyone else. I weighed my options and went with a succession of short term policies (~200/year for catastrophic coverage and no pre-existing coverage), on the theory that I was healthy but for this rare pre-existing condition and the worst that could happen was that my pre-existing condition would act up, I'd have one big splash when I was hospitalized, and then I'd have to buy into the open enrollment at several times the cost my daughter would have to pay.
Since then (99+), I have had coverage through work - sometimes at the cost of my emotional health - staying at my most recent position far longer than it was emotionally healthy because it was the only option for covering my entire family. Our options were - put up with an emotionally unhealthy job, or pay whatever the insurance company felt like charging us under COBRA, then the HIPAA conversion to individual coverage.
I recently switched jobs - taking a 60% pay cut (and worse health care benefits) because the job is better for me emotionally and still provides coverage for all of us.
But my daughter would have been off my health insurance 4 years ago because she cannot manage a full time load at school or work, and we would have had to get her on disabilitiy, but for the ACA. She now has the option, because of the ACA, to be a starving artist and not have to work toward a job she hates because it is the only way she can survive. Her billed medical costs are $60,000 in a good year. She literally cannot survive without the ACA.
So I have very little patience with people with similarly devastating conditions, who don't pay enough attention to take advantage of the system and then blast the system which is far from perfect ** but which offers life to people like Will's wife and my daughter. Because blasting it gives ammunition to those who want to destroy it and replace it with nothing.
What the ACA offers is worlds better than what we had before. *All* we got in the last major reform (~1996) was HIPAA individual policies (with unlimited premiums) available only to those who had a job and left it, and *all* we got the time before that (~1980) was COBRA - 18 month policies again, unlimited premiums and only available to those leaving jobs where they had had health insurance. My daughter can't live for another decade and a half waiting for perfection, just because the major reform we got this time isn't anywhere near perfect.
questionseverything
(10,654 posts)the language was there.....
are you saying the ins paid for meds not covered in contract?
now if you were arguing over what is "reasonable and customary" then yes there is contract language that state ins department could help with
but if you are saying you got something covered that was not in contract......I call bs
without knowing what will has in his contract's language, it is impossible to tell
Add to Journal Self-delete Edit post Reply to this post
Back to top Alert abuse Link here Permalink
--------------------------------------------------------------------------------
Response to questionseverything (Reply #263)
Tue Mar 18, 2014, 09:20 PM
Star Member Nye Bevan (14,816 posts)
273. My policies (and I believe most policies) have "non-formulary exception" provisions
with this kind of language:
Non-formulary exception process
The non-formulary exception process provides physicians and members with access to non-formulary drugs and facilitates prescription drug coverage of medically necessary, non-formulary drugs as determined by the prescribing practitioner.
Patients can also have a non-formulary drug without invoking the exception process anytime by paying full price for the drug if the prescribing provider deems the non-formulary drug not medically necessary, but agrees to prescribe the drug due to patient demand.
The prescribing practitioner makes the final decision regarding what drug is appropriate for the member. Non-formulary drugs should be used only if the patient fails to respond to formulary drug therapy, has an adverse reaction to formulary drug, or has other special circumstances requiring the use of a non-formulary drug.
////////////////////////////////////
I would like to address this quote of yours..
Because blasting it gives ammunition to those who want to destroy it and replace it with nothing. //////////////////////
pointing out problems is the only way to fix them.....I have never seen any1 on du say they wanted to repeal aca only that we want it expanded and costs lowered
Ms. Toad
(36,471 posts)Lovenox (subcutaneous heparin) was excluded from coverage for any use other than pre-treatment for surgery. I gave you several links which described what was going on at the time. The vast majority of people who tried to obtain coverage (under any policy) to use it to treat DVT were denied because it was excluded from coverage. At least one of the articles I linked to mentioned this and, as I said, the TV show ER had an episode within a year of my encounter with the standard outcome - the coverage was denied and the patient had to be hospitalized for 5-10 days (standard treatment at the time) when it would have been a whole lot cheaper to pay ~$500 (at the time) for a Lovenox prescription.
My doctors were successful in advocating for me to get it covered, even though it was excluded from coverage.
This was before formularies played a significant role - so it wasn't a matter of getting an exception to the formulary. It was also, under my plan, classified as medical care (rather than prescription).in connection with a single permitted use. One of the articles I linked to mentioned this weird coverage split (prescription v. medical).
As to wanting to repeal the ACA - there are plenty of folks on DU who want to see it abolished. They want single payer, but in the mean time they want the ACA gone. And rants like the one which started this thread aren't helpful.
bullsnarfle
(254 posts)Come on down and try that in Florida, pal. This place is run by Gov. Voldemort and his minions. Remember him? He CEO'd a crooked health insurance company (like there is any other kind), walked away with a platinum parachute, and used the ill-gotten gains to buy the governorship. He and his cronies own this state. Letters and bitching will get you exactly SQUAT here, dude.
Others have said it on this site, and I will reiterate - Access to health insurance DOES NOT equal health care. You can pay, and pay, and pay, and when the time comes for insurance co. to pony up they just...don't pay. Hey, the doctors may be sympathetic, but they want their money, and if they can't get it from old Double Cross they will go after you. I mean, what are you going to do, hire a lawyer? Bwahahahahahaha...yeah, right.
wordpix
(18,652 posts)If they're Dems, that is, they will act to help you.
If they're repukes, all bets are off
thesquanderer
(12,550 posts)As I understand it, for individual insurance purchasers (which it sounds like you are), grandfathering allows--but does not require--you to stay with a pre-ACA plan that you already have, if you like it better than getting a new ACA plan. Most people are probably better off with an ACA plan, but grandfathering is there for the rare exception, or for people who are just scared by the idea of changing to something new. I think you should definitely check into the ACA plans in your state right away and see what your options really are.
Obamacare is not forcing your old insurance company to deny you anything... they would have denied you the same thing before Obamacare existed. After all, grandfather means it's the same plan it was before Obamacare. But at least in theory, Obamacare gives you new, better options that you didn't have before. It's worth trying to find them.
pnwmom
(109,801 posts)We were also working with an independent, whose emails to us had boilerplate on them about having to get approved to get the insurance. I finally asked about this, and he acknowledged that the law was changing as of January 1, 2014 so that they would have to take every customer, without regard to preexisting conditions.
But their email boilerplate still had the false information after Jan. 1. We ended up buying through the exchange. But another option might be better for you -- just not with your uninformed friend.
http://www.nytimes.com/2013/10/26/your-money/health-insurance-options-arent-limited-to-obamacare-exchanges.html?_r=0
In general, health policies effective Jan. 1, whether sold on the exchanges or off, must comply with the Affordable Care Act. That means they have to offer the same menu of essential benefits, like drug coverage and maternity care, and can’t deny you coverage if you’re already sick. And, insurers who sell policies both on and off the exchanges must sell the same plan for the same price.
http://www.insure.com/articles/healthinsurance/buying-health-insurance-outside-exchange.html?WT.qs_osrc=fxb-182807210
Drug coverage
Drug coverage is yet another variable. You may find you have more options when it comes to drug coverage if you shop off-exchange. Like provider networks, health plans can limit the drugs that are covered, or reimburse more for generics than brand-names, or reimburse more for drugs you buy mail-order than from your local pharmacy.
If you have a health condition and use a particular drug, you should check that it's covered under the plan in which you want to enroll, whether that plan is on the exchange or off-exchange, Coleman advises.
Remember, too, he says, the cap on out-of-pocket expenses doesn't apply to drugs not on a health plan's list of covered medications.
Nye Bevan
(25,406 posts)But as you point out, the same rules apply to these plans in terms of guaranteed issue regardless of pre-existing conditions, no out of pocket costs for preventive care, and so on. And at least where I live, the off-exchange plans have vastly superior networks of doctors than the exchange plans.
Response to WilliamPitt (Reply #8)
Name removed Message auto-removed
Zorra
(27,670 posts)insurance companies.
So very sorry for this massive injustice that has been done to your family, Will.
"Fascism should more properly be called corporatism because it is the merger of state and corporate power." -- Benito Mussolini
truedelphi
(32,324 posts)To begin?
Brigid
(17,621 posts)But I fear it won't happen. I support ACA because -- and only because -- I want it to be a first step towards single payer. On its own, it is little more than a huge giveaway to the insurance companies and Big Pharma.
Doctor_J
(36,392 posts)I have only 20 years or so to go, and it will be at least 50 before we decouple Big Insurance from the government, if at all.
C_U_L8R
(46,924 posts)Heard of this but never tried it...
http://familywize.org
loudsue
(14,087 posts)if people are FORCED to buy insurance, then at least the insurance companies should be FORCED to cover keeping people healthy.
Egnever
(21,506 posts)Seems pretty foolish.
bvar22
(39,909 posts)...and in this case it is beyond rude.
being a victim is beyond foolish. Especially where your health is concerned.
If you need a medicine to live and you cant be bothered to check if it is covered by a plan you are thinking about purchasing you aren't a victim you are a fool.
That's like buying a Prius and claiming to be a victim when you cant tow your boat with it.
Much easier to blame others for your own indifference though isn't it?
questionseverything
(10,654 posts)http://www.bcbsil.com/PDF/rx/rx_list_std_il.pdf
Specialty drugs
Specialty drugs are used in the treatment of medical conditions such as hepatitis, hemophilia, multiple sclerosis
and rheumatoid arthritis. Specialty drugs may be oral, topical or injectable medications that can either be
self-administered or administered by a health care professional. For a current list of specialty medications,
visit myprime.com or bcbsil.com and log in to Blue Access for Members.
Note that some drug classes may be excluded by some plans and therefore may not be covered under your
pharmacy benefit. Your plan may have a different coverage level for self-administered specialty drugs. If you
have questions about your coverage for specialty medications or your prescription drug benefit, call the
number on the back of your ID card.
////////////////////////////////////////////////////////
how do I look it up before I buy?
I have to be a member before I can see the list
cimzia is what I am looking for
steve2470
(37,468 posts)sinkingfeeling
(54,845 posts)of the utmost importance that people check the drug formulary for the plan they are about to chose. This is the same thing people who are dependent on a certain drug must go through when they select their Medicare Part D provider. My mother has had to change her providers several times due to changes in her prescribed medicines and one can only do that by looking at the formulary and the tiers of drugs.
Here's an example from Anthem:
https://www.anthem.com/shop/content/olspublic/pdf/2014/english/MAPD_ComForm_Acc_Val_OH.pdf
questionseverything
(10,654 posts)specialty drugs can not be checked on BEFORE you buy
after you buy you can be denied and appeal and denied and re appeal....all while paying enormous premiums ...lucky us!!!
I remember some guy that said,
I watched my mother fighting cancer, dying and trying figure out insurance company forms from her hospital bed....time she should of been able to spend with her grandchildren and her loved ones
as a nation we embraced that guy and gave him a mandate to change that system but for many we are right back where we started except now no matter how badly insurance acts ,it is by law mandated
LiberalEsto
(22,845 posts)Either that, or single payer.
At the very least, we need to be able to look up their formularies before signing on.
Can the Consumer Financial Protection Bureau do something about this, or is it out of their jurisdiction?
sinkingfeeling
(54,845 posts)Here's the one for Anthem BCBS:
https://www.anthem.com/health-insurance/nsecurepdf/pharmacy_NatlAccts_Specialty_DL
questionseverything
(10,654 posts)it says after you have PAID you can ask (beg) the insurance company to let you receive the drug
and they can change it at will according to your link>>>>>
This list may change without notice which may affect your benefit coverage.
sinkingfeeling
(54,845 posts)are available under all policies. Special drug lists require special things, like using a tier one drug before being allowed the tier two drug or being pre-approved for the drug by the doctors, or using one brand name instead of another, or having a limit on the amount of the drug you can receive. That's why they're on special drug lists.
Honestly, this stuff has been round since Medicare Part D kicked in. In the case of ACA, the states got to chose how participating companies 'picked' the drugs to be in their formularies.
questionseverything
(10,654 posts)before he bought his plan
I posted a formulary to show ,they do not promise to cover certain drugs before you buy...you can only apply after you have paid
your argument seems to be it was always like this and I would agree with that but that does not make it right
Ms. Toad
(36,471 posts)is tied to particular plans. The link (and quote) does not say that you cannot find out ahead of time which specialty drugs covered on a particular plan, it says you have to log in to see it online, because what is covered is tied to a specific plan. Have you tried calling, telling customer service person and asking about the plan you are interested in buying, to see whether the drugs you are concerned about are covered?
I have never, on any plan where there was a formulary or a specialty drug list, been denied that information in advance of purchasing the plan. The last time was October. In order to answer my question about a medication in a class that is frequently not covered (and often not listed in formularies), the person on the phone had to find someone on the plan I was considering who was getting that medication to confirm it was covered, and at what price - since it was plan specific. But she found and provided the information to me - as has happened with each of the plans I have had over the last several years.
It is far more effective to find the customer service number and call and ask, than it is to complain on an internet board (which they will never read) that they won't give you the information.
Response to questionseverything (Reply #610)
REP This message was self-deleted by its author.
Ms. Toad
(36,471 posts)The last 4 plans I have been on have had a specialty drug category - and in each case I was able to check the coverage and price I would be charged. They cannot, of course, tell me whether an appeal of something which is not part of their formulary or specialty drug list will be approved prior to purchasing the plan - since that is based on unique medical circumstances. But they can (and in my experience always do) tell you the list if you ask.
And, FWIW, I have never lost an appeal (we are billed $60-100,000 a year - so you can imagine I have lots of encounters over insurance issues). In my 30 years of dealing with insurance companies, I have decided not to pursue two claims - out of network co-payment for an air cast which I would have had to drive 100 miles to find in-network, and authorization to see a pediatric (as opposed to adult) orthopedic specialist in connection with a break near a growth plate. Both were related to a doctor I fired for her refusal to assist in the corresponding appeals. I have been successful in obtaining approval for 2 experimental treatments (one surgical, one pharmaceutical), access to numerous step therapy treatments, in network treatment for costly care by an out of network specialist, family coverage for our same gender family (at a 30% reduction in out of pocket expenses) - and many more.
I agree - it should not be so hard, and it has robbed time I could have spent being present for my ill family members. But information, and successful appeals, are possible.
Control-Z
(15,686 posts)and then compare each and every plan's coverage of those drugs before I purchased.
Hissyspit
(45,790 posts)Yeah, sure. People just love to get scammed. Read your sentence. It doesn't even make sense.
"Much easier to blame others for your own indifference."
What indifference are you talking about? They've been working on this for months.
And this is JUST like buying a car to tow a boat. (Of course, now that you mention it, car dealers have a long history of being dishonest, unethical scam artists.)
JEB
(4,748 posts)as the heartless lying thieving scum they are. After 45 minutes on hold..."this conversation will be recorded..." FOAD
Boudica the Lyoness
(2,899 posts)in the future.
Thank you.
bluestate10
(10,942 posts)If a patient insists on a particular medication when other therapies will work that mindset helps NONE of us. I don't know the details of the OP's wife's situation, but I do know that I had three medications that worked for a situation that I had, my plan gave me a choice and I chose it's default, which was the least expensive choice, I am doing perfectly fine with the alternative.
lapislzi
(5,762 posts)The PATIENT doesn't insist on the medication. Last time I checked, it was the doctors that write the prescriptions, and how fucking DARE a bean counter who wouldn't know how to put a stethoscope in his own ears presume to tell the patient with a life-threatening condition what medication she should be on.
While I am happy for you that you are doing well on the medication that your insurance company chose for you, you have absolutely no business telling others what medications they ought to try.
uppityperson
(115,920 posts)problem. Insurance companies do not have prescriptive authority in any state I know of, and often other therapies do not work, like in the case of Will's wife.
Zorra
(27,670 posts)
(Post #9 added to the top ten list of things that make DU suck.)
Egnever
(21,506 posts)only a failure on Wills part to check their formulary. The insurance company will provide that to anyone that requests it, They have to by law.
bvar22
(39,909 posts)and if you do, hey great!
..but not everyone is skilled or educated in the ability to see through all of the tricks played on the average American by the Health Insurance creeps.
Do you happen to work for one?
Is that how you know all those words like "formulary".
I only have a Masters Degree,
and have never heard of it before.
YES.
You ARE blaming the victim,
and using this to put on a little arrogant performance about how SMART you are.
It is like Steve Jobs saying
Hey. I built a computer and made a Billion Dollars.
You should do that too,
and if you don't...thats just your own damned fault.
You should be ashamed,
but, somehow, I doubt you can experience that feeling.
<expletive deleted> You!
Response to bvar22 (Reply #126)
Post removed
bvar22
(39,909 posts)I should be able to check ALL the fine print in ALL of the policies offered in the Exchange while negotiating through Healthcare.Gov Website... or talking on the phoen with a representative.
![]()
How many people who signed up through The Exchange even got a look at their policies?
I think that maybe ZERO could be the right answer.
How do you check the "formulary" over the telephone?
I STILL haven't seen a hard copy of MY policy.
You DO know that in civilized countries,
NOBODY has to do those things?
Yes?
I am not the one calling Will an idiot,
because I signed with an Insurance Company without checking the "formulary" either,
along with several MILLION other Americans.
YOU are the one calling Will and Me and MILLIONS of others idiots.
Well, GOOD for YOU!
This is supposed to be The Affordable Care Act.
and The Exchange was for people who previously were unable to afford Health Insurance.
How many people out of THAT pool of MILLIONS do YOU believe know the meaning of the word "formulary",
much less have the ability to check the Prescriptions, or even pronounce the names of those prescriptions?
YES.
You ARE blaming the victims.
MILLIONS of them.
This particular problem will NOT be limited to Will.
I can't print the words I feel that describe your
Well, everybody should just be as smart as me
smug, elitist, above it all, blame-the-victim attitude.
That is usually reserved for Ultra-(Its your own damned fault)Conservatives and the I Got MINE, FU libertarians".
JEB
(4,748 posts)Enthusiast
(50,983 posts)Response to bvar22 (Reply #258)
Name removed Message auto-removed
Zorra
(27,670 posts)evasion, bait and switch, and fine print down to an exact science. Checking the formulary of an insurance company is not always easy, especially after you've been totally beaten down dealing with deliberately insane bureaucracies who eat up most of your spare time when you are just trying to get straight answers from them.
It took me 63 days of intense frustrating, mind numbing struggle in overcoming built in programmatic stupidity to get my insurance plan through the ACA, through no fault of my own, and once I finally got approved for a plan, I was not permitted to examine the overwhelming majority of the details of the plans available to me before I chose one.
Fortunately, I got lucky, and my plan seems to be a good one. However, they apparently deceived my optometrist into believing that they would pay for my thorough eye exam; the optometrist told me the insurance company would pay, and after the exam found out that they were not getting paid. But the optometrist was honorable, and did not require me to pay, and just ate the cost of my exam, because they acknowledged that had told me my insurance was going to cover.
People should not have to go through all this deliberately deceitful, complex maze of crap devised by profit seeking businesspeople whose job it is to rip people off in any way possible in order to receive health services and health insurance benefits.
It sucks, it's evil, and I aim to help destroy the private health insurance industry as quickly as possible by any non-violent means necessary.
Egnever
(21,506 posts)Even more so when you have a drug you depend on.
I am not claiming insurance companies are benevolent but the formulary is one thing about them that is black and white. If you dont check it when you are purchasing a plan and there is a drug you need covered you are not a victim.
TrollBuster9090
(6,053 posts)to be effective. (That's even true in countries with a single payer health care system.) And, if you're talking about a drug that IS proven to be effective, but there are several brand name formulations vs. alternative (generic) equivalents that are proven to be as effective (or in the same ballpark) an insurance provider is free to say you have to use the cheaper one. A problem sometimes arises when somebody is used to a brand name that is five times more expensive than the generic version; or has been using a more expensive formulation that hasn't been proven to be more effective than an alternative, cheaper formulation with the same active ingredients.
That happens all the time; but it's not really a denial of a life-saving medication. It's just a denial of a more expensive version of something that isn't proven to be more effective that some other treatment.
I don't know if that's the case here, though. I'm just saying there's a lot of noise about this kind of thing that goes on whenever people are required to switch plans or providers. And it happened long before the ACA.
Zorra
(27,670 posts)truedelphi
(32,324 posts)I am firmly convinced that many of those exonerating or even praising the ACA are younger and healthy and are probably not going to have to actually use the system for quite a while. Or else they re people who are on a premium plan, through an employer or through being able to afford such.
But for people who have to use an insurer that is offering them less than a premium plan, there is a lot of bitter to have to suck on.
Considering the fact that the guy occupying the Oval Office and the Dem majority that had both houses from Jan 2007 to Jan 2011 had continually put out there the possibility of a public option, only to retract such once pressured by industry, it is natural that people are disappointed and if denied coverage like essential meds, even damn angry. There should have been a lot more reform and a lot less in terms of loopholes and give aways to the Big Insurers.
But the Beltway whores are what they are.
freebrew
(1,917 posts)People w/ certain jobs have 'premium' health plans. The company they work for probably pays a lot of premium for these plans, maybe. If you're getting a subsidy and so getting a 'cheaper' rate, this subsidy is coming from taxes. The insurance company is still getting top dollar for these less than premium policies that should be just as good or better than those so-called premium plans coming from employers.
Anthem can certainly afford to pay for Will's wife's meds. I've been through similar experience and for some reason, the insurance companies would rather be assholes about it. But, from what I've seen, these fights always end up costing the insurance companies more than if they just listened to the Doctor.
Cha
(309,260 posts)them.
bluestate10
(10,942 posts)magical thyme
(14,881 posts)when YOU ARE REQUIRED TO SIGN UP IN ORDER TO SEE THE FORMULARY
and then it states that your particular plan may not include all the drugs in the formulary
is a lot of things. A valid observation is not one of them.
Zorra
(27,670 posts)don't have a clue as to why the post is so utterly offensive to Democrats and other progressives.
Plus, Pretzel_Winger and his right sock got tombstoned today for engaging in the typical RW behavior of cheating.
PowerToThePeople
(9,610 posts)MoonchildCA
(1,344 posts)There is limited information on our state site, as well. You can only get the most basic information on what is covered. You can't call--they are overwhelmed and no one answers. My friend signed up for Anthem Blue Cross because she had them before and was familiar with them. She found out, only after she signed up (because you have to be a member to have access), none of her doctors are in her network--doctors who previously took Blue Cross. in fact, the nearest oncologist is 20 miles away, and we do not live in a small town. we have two hospitals here, and neither is in her Network.
She and I both already had "Obamacare." We went from the California Pre-existing Insurance Plan (the absolute best thing ever!), to the Federal pre-existing Insurance Plan (not as great, but adequate), and have now had to transition into the exchange. She has been in pain management for years, and it took her over a month to finally get those meds approved. Her pain management doctor was the only one in her network. He accepted the copay, but now she is being billed for the entire amount--over $200. In-network doctors should only cost the copay. There is no one to call; nobody answers.
She was not sent a booklet on coverage (like our former insurances did). Basically, you're just left out in the cold to navigate it yourself. You really don't know if something is covered until you get a bill.
My husband and I signed up for Blue Shield. We haven't attempted to use it yet, but I'm really stressed after what my friend has been going through.
And full disclosure: I am only alive because of Obamacare. I needed major surgery in 2012; I signed up for CA Pre-existing Insurance Plan, and received a $300,000 dollar surgery the next month. I was prepared to LOVE the exchanges...
itsrobert
(14,157 posts)What if my medicine isn't on a plan's formulary?
If you can't find your medicine on a health plan's drug list in your state's Marketplace, you can request that your plan cover it or give you access to it.
You can request that your insurer cover a medication not on its formulary with the help of your doctor to explain the medical need. If your request is denied, you have the right to appeal your health plan's decision.
http://www.webmd.com/health-insurance/insurance-costs/aca-prescription-drug-costs-faq
Whisp
(24,096 posts)itsrobert
(14,157 posts)Why not pursue all angles before the "anger" is posted?
truedelphi
(32,324 posts)A Rahm/Liz Fowler extravaganza, no one would have to spend any of their time appealing any thing.
At some point in your happy go lucky life, you might need to use your health insurance. And then you too will get to find out what it is like to have to go without a treatment you need, or a medicine that is essential, due to cost. All the while having to spend hours of your life, that should be being spent productively, dealing with Big Health Insurers.
theboss
(10,491 posts)He do what he do.
treestar
(82,383 posts)leave out a specific medication in a specific case? We are still dealing with insurance adjustors, and people may not like that, but that's what we've got.
And we can't prove single payer plans don't have bureaucratic glitches too.
Hoyt
(54,770 posts)And, the drug coverage is subject to even more restricted formularies.
bluestate10
(10,942 posts)The emotional part pleases some on DU, in particular when the President is targeted, but the emotion doesn't make the claim true. I suspect that there were effective alternatives offered and they were rejected, in such a case even the best plans will reject prescription fills.
Hekate
(97,014 posts)What we have is a generic "Fuck Obama he's teh evil" post, and I for one have a hard time parsing out what actually happened and what alternatives were tried.
I do know that my husband reads his company-offered insurance plan's fine print every year so there will be no surprises.
We've known what a formulary is for at least 25 years, because some of our meds (especially mine) are routinely denied every single year. My primary doc is sick of countersigning the letter I keep on file in my computer testifying in excruciating detail what side effects are caused by my taking a particular cheap generic, but I print it out and he faxes it from his office with his own note. Every year.
If at first you don't succeed, keep trying. Keep notes in a file, with dates and contact info.
I'm going to get put on ignore for this, or flamed, but the OP married a woman with a severe, chronic, and progressive disease. My sympathies are with them both. But it means he signed up for a lifetime of reading the fine print and doing the research. I wish them both all the best, but Obama is not teh evil because of it.
SidDithers
(44,331 posts)Sid
wickerwoman
(5,662 posts)Only because he lives in America which, last time I checked, doesn't have a sign up sheet. If he lived in a number of other countries, he and his wife would just go to their doctor and get care.
I have absolutely no idea what a "formulary" is. If I get sick, I don't run to the internets and start shopping for a health insurance plan or researching which medications are covered among dozens of "options". I go to the doctor and get what I need.
But then I live in a country that actually gives a fuck about helping people instead of squeezing every last dime out of them and then blaming them for being broke and sick and tired and too busy to read dozens of pages of fine print specifically designed to screw them over.
What are the hundreds of millions of Americans with below average intelligence or learning disabilities or ESL issues or overwhelming stress from poverty and working three jobs to scrape by supposed to do? Suck it up and believe that they are the problem, not a system that doesn't give a shit about them and is intentionally designed to disadvantage them?
Hekate
(97,014 posts)...with none of the disabilities you list. He has become progressively more enraged at Obama's perceived perfidy, and it has caused him to blame everything, including his own decisions, on Obama. I've been reading his posts and essays for nearly 12 years, and he's shared a lot about his life on this board. I'm sincere in my sympathy for him and the woman he loves -- but I am not sympathetic to this latest screed, because as far as I can tell he is working backward from a foregone conclusion.
Saying there are "hundreds of millions of Americans" simply unable to cope with the best President Obama and the Dems were able to cobble together given the intense opposition they face is rather overstating the case. If that were so the entire population of the US would be covered by your blanket statement.
I don't know what paradise you live in, but you are not in possession of all the facts about what we are trying to do here, where we live. You are taking the frustrations of some folks on one discussion board -- and in particular one man -- as if they were the whole story, and they are not.
There are a lot of DUers who would like to brainstorm ways to help the OP through this trying time. However, given the progression of his rage at Obama, I am not optimistic of the outcome.
wickerwoman
(5,662 posts)and I left specifically so I wouldn't have to deal with this kind of shit. I still have family who are going through it and I thank my lucky stars every goddamn day that I don't have to. Emigrating from the US was the single best decision of my entire life.
This is not an issue which is specific to one person and brainstorming ideas to help Will through this one particular crisis misses the point. He's pissed off at a broken system and he has every right to be. Telling him that it's ever so slightly less broken than he is making out (while also suggesting that the burden should be on him to navigate it) is not helping either him or the larger problem.
truedelphi
(32,324 posts)At a puppet, even a puppet that occupies the Oval Office, was a bit of a waste of time.
Humanist_Activist
(7,670 posts)for non-medical reasons(i.e. medication is too expensive). By which point the appeals process will eventually be exhausted.
itsrobert
(14,157 posts)It doesn't hurt to appeal. Nobody said it has to be approved. I must of missed that part.
Humanist_Activist
(7,670 posts)went through the appeals process, and were ultimately denied.
After that point, you are SOL unless you can get some type of charity or government help.
itsrobert
(14,157 posts)other that he wants to fuck the President and thinks the President is a used car salesman.
treestar
(82,383 posts)But wouldn't get credit for medications approved immediately! Naturally. Nobody like to fight with insurance companies. But then who is to say even single payer would not result in this type of fight? The government might claim a medication not needed where patient and doctor disagree.
itsrobert
(14,157 posts)but there is an appeals process and my wife was able to get the medication her doctor recommended.
TheKentuckian
(26,314 posts)They have the simplest criteria and formulary is easiest get an override on. As far as I can tell, if you have a condition where it is generally agreed that a treatment is effective then it will be covered with little mess at all.
Off label and experimental applications, you may have some trouble but FDA approved comparably simple compared to most.
I suggest Will approach the manufacturer for help, that is often the last line of defense nowadays but you generally will have to be in a situation where they will not cover a formulary alternative for you either.
There are some charitable foundations but funds are very limited because they have been hit up hard for the past few years.
Is this Obama's fault? Of course not.
The problem is of course these maddeningly stressful, quality of life, and even life and death issues were not taken from our plate and this is because mostly we do not have systemic reform but rather what we actually did was really more closely align the individual market with the large group market and improve access via a hodgepodge of approaches in exchange for guaranteed customers and a mainline to the treasury so the deal is over sold.
A lot of people looking for relief will find none, we have the same system as before with some curbs on SOME of the roughest edges. This has turned out to largely be standardization, which is a good thing because the individual market was fucking Thunderdome crazy town but it is still very ugly.
Satisfaction with large group plans is driven by lack of use and employer subsidy, folks that have to use it tend to hate it almost as much as individuals because of the hell they put you through and the costs start to show up beyond premiums and copays.
Humanist_Activist
(7,670 posts)and the institutional stagnation of it means that the ACA was going to be a compromised compromise that isn't going to solve most of the problems it claims it can solve. Barring an outright revolution, or radical cultural and political shift, we aren't going to see our private/public system fixed completely in probably another generation or two. The ACA may be a good first step, but it isn't the end all, be all of health care reform.
lumpy
(13,704 posts)JoeyT
(6,785 posts)Some Important Details
The parts of the Affordable Care Act that concern internal appeals and external reviews apply only to health plans or policies that were created or purchased after March 23, 2010. Plans created on or before March 23, 2010, may be “grandfathered health plans.” The appeals and review rights do not apply to them.
Edited to add: Which is sort of confusing. In one place it says created or purchased, in the other it just says created before may be grandfathered.
MannyGoldstein
(34,589 posts)to not give me $100 million.
How do you think I should spend the money?
itsrobert
(14,157 posts)Are prescription drug plans the same in every state?
No. All health plans in a Marketplace must include prescription drug coverage, but each state sets the list of covered medicines, called the formulary. For instance, one plan may have many more medicines in one category or class than another state does.
http://www.webmd.com/health-insurance/insurance-costs/aca-prescription-drug-costs-faq
Baitball Blogger
(49,642 posts)There were loopholes with the early HMOs too. We need to work together to get this information out to the executive office. I bet we can make a difference.
itsrobert
(14,157 posts)How do I know if a health plan will cover the medicines I take?
Check the plan's formulary, also known as a preferred drug list. You should be able to get this from any health plan you're considering. Sometimes a plan's formulary will be on its web site.
The formulary lists each brand and generic name of medicines that the plan will help pay for. To look for your medicines, you need to know:
•The medicine's exact name
•The dose you take
•How many pills your doctor usually prescribes
http://www.webmd.com/health-insurance/insurance-costs/aca-prescription-drug-costs-faq
bvar22
(39,909 posts)What about the medicines I might need next year for a condition I haven't yet developed?
In civilized countries, they don't have to do that.
progressoid
(51,186 posts)Who wudda thunk it.
We also have "coverage". But we don't use it because it's too expensive. We're basically shelling out cash in the hopes we are covered for any catastrophic problem.
marzipanni
(6,012 posts)not for a bunch of people sitting in cubicles trying to figure out ways NOT TO PAY for health care!
Will, appeal that decision!-
http://www.hhs.gov/healthcare/rights/appeal/appealing-health-plan-decisions.html
progressoid
(51,186 posts)80% of what insurance companies collect is supposed to go to the provider. But that's after the co-pay and the 7800.00 deductible. Then 80% goes toward health care.
It's not the Afordable Care Act. It's the For-Profit-Insurance Act.
Recursion
(56,582 posts)80% of insurers' revenues must go to treatments. If less goes, they have to cut refund checks to policy holders (this has already happened several times).
Plans are are required to, on average, pay 60, 70, or 80% (depending) of their pool's total medical costs. The deductibles are how they get there.
progressoid
(51,186 posts)I'm paying deductible out of pocket before my insurance company will begin to pay for treatments. 80% notwithstanding.
Recursion
(56,582 posts)There are plans with low or even no deductibles, but their premiums cost more. It's a question of which one makes better sense for you.
Whisp
(24,096 posts)disgusting.
Response to WilliamPitt (Original post)
Name removed Message auto-removed
itsrobert
(14,157 posts)Did you not look at the covered medications of that plan before you selected it? Especially if that medication is important in a family's members survival? Have you appealed the insurer's decision?
TBF
(35,069 posts)itsrobert
(14,157 posts)Trying to find out what went wrong here so others can learn. And to see if all avenues have been exhausted prior to posting this "anger". Maybe there is something that was missed, that may help.
thanks!
TBF
(35,069 posts)well, Repugs are that stupid - but most people are not. They know when they are being screwed. Mr. Pitt's anger, granted, is basically misplaced. I agree with him on so much - but I think he doesn't go as far as we need to. I believe he still sees capitalism as salvageable given progressive governing.
I don't see POTUS as the real problem. He's functioning as expected by the folks who hired him.
The underlying problem is an economic system in which things like health care are for-profit. Capitalism has to go.
Lars39
(26,351 posts)one_voice
(20,043 posts)WilliamPitt
(58,179 posts)My post #8 above:
There are ten different health insurance companies in NH. According to the independent (family friend, ally) insurance adjuster I spoke to at length this afternoon, pursuing coverage with any of them would be a waste of time. Why? Because - according to dude - the whole "You cannot deny coverage to people with pre-existing conditions" thing only applies to insurance companies within the ACA network. You heard all that shit about "Grandfathering." Well, this is that, and all of them will turn us down because they still can.
I am in the process of running down the facts of the matter, but family friend and ally was confident enough to basically tell us not to bother.
So yeah, that, too.
Explain it away, apologist. My wife is counting pills.
uppityperson
(115,920 posts)be able to rebut an argument by doing more than insult. And yes, I am aware I kickedyour thread, hoping others see how you insult President Obama.
bluestate10
(10,942 posts)as the OP. Our state's medical environment is dominated by big HMOs and Doctor collectives. I am a member of one of the biggest Doctor collectives in the state and am covered by one of the largest HMOs. I have yet to see a situation where prescriptions were denied when people were using within what health maintenance models indicate keeps the person healthy. If patients do have to pay, they only pay for the prescription fill that goes out the model, once back in that model, the prescription is free or comes at a vastly reduced price. I am younger, but my plan is loaded with elderly people, many cancer patients, I have seen no one complaining about being denied needed medication or being bankrupted to pay for medication.
okaawhatever
(9,560 posts)is an answer to this that perhaps hasn't been presented.
Cha
(309,260 posts)fault. That doesn't matter.. what matters is..

Yeah, Kicking the Thread..
one_voice
(20,043 posts)Last edited Tue Mar 18, 2014, 06:18 PM - Edit history (1)
I really do.
I'm on disability and take VERY expensive meds. I've had to go without because I didn't have the money. I think we should have universal health care.
You know nothing about me and yet you insult me calling me an apologist. I'm not, I just think we should be better than the other side.
While your wife is counting pills, I'm going on two months without one of my most important meds. Today my doctor gave my husband samples of his diabetes med to get him through till our insurance goes into effect.
Not liking how you expressed yourself is NOT the same as being an apologist.
I truly hope you get this worked out---NO ONE should go without meds---I know, I'm doing it.
Orsino
(37,428 posts)And had he written it more to our liking, Congress would not have passed it.
marble falls
(64,371 posts)are covered by ACA but those already denied will continue to be denied as grandfathered by earlier denial? How haven't we been told this before by the "liberal" press?
uppityperson
(115,920 posts)DU Community Standards, I just don't know about this place.
WilliamPitt
(58,179 posts)Yet.
Cope with a different opinion.
ProSense
(116,464 posts)I mean the attack seems purely gratuitous.
It's your responsiblity to check to see if your medications are covered. This was true before the ACA.
The fact is that you can work with the insurance company to see if they will cover it, and you can appeal their decision.
treestar
(82,383 posts)Who won't do what you want right away. But the POTUS is not the first person I'd think of. Just weird.
Cha
(309,260 posts)there he is.. calling the President all kinds of stupid juvenile names, stomping his feet, and raging at Pres Obama.

Lydia Leftcoast
(48,219 posts)meeting with them behind closed doors to ASK them what they were willing to do (sort of like Dick Cheney meeting with the oil companies), Will's wife might not be in this position.
ProSense
(116,464 posts)They exist in Medicare Part D.
Being uninformed is not an excuse to attack the President.
Lydia Leftcoast
(48,219 posts)to the extent of denying people the meds they need to half a progressive disease.
Either way, those closed-door meetings with the insurance companies stink to high heaven.
Governments are supposed to tell private businesses what they can do, not the other way around.
Who but major corporations gets to tell the president and Congress which potential laws they are willing to follow?
Oh, and the pharmaceutical companies deserve a hearty "fuck you" as well for profiteering in the only country in the Western world that doesn't regulate drug prices.
And no move to reform Medicare Part D completely instead of just shrinking the doughnut hole? No reforms that allow Medicare Part D to negotiate drug prices?
ProSense
(116,464 posts)"True, formularies existed, but that doesn't mean they SHOULD exist"
...bizarre thing about attacking the President and Obamacare is that the law did improve the situation.
The Affordable Care Act ensures your right to appeal health insurance plan decisions--to ask that your plan reconsider its decision to deny payment for a service or treatment. New rules that apply to health plans created after March 23, 2010 spell out how your plan must handle your appeal (usually called an “internal appeal”). If your plan still denies payment after considering your appeal, the law permits you to have an independent review organization decide whether to uphold or overturn the plan’s decision. This final check is often referred to as an “external review.”
http://www.hhs.gov/healthcare/rights/appeal/appealing-health-plan-decisions.html
Recursion
(56,582 posts)Neither does a system like the ACA.
The only way to not have formularies is to nationalize pharmaceutical production, though that ends up just being formularies by another name, since then the government is deciding what drugs to make when.
SidDithers
(44,331 posts)That's why many of us have Extended Health Benefits through our employers, which covers Dental, Vision and Drugs.
For large expenses, people can apply to their Province for drug coverage (Trillium Foundation in Ontario), and seniors get drug coverage when they hit 65. For the rest of us, we're on our own.
Sid
bluestate10
(10,942 posts)detailing all facts. I happen to live in the same sate as the OP live in or lived in. I know how health maintenance in my state works, and my plan has a large percentage of seriously ill or aged people - FUCKING none have complained about being bankrupted to pay for or denied needed medication. The predictable amen chorus cheered the OP on, probably because of what the OP called a President who has been a honest actor on health care reform.
1StrongBlackMan
(31,849 posts)a President TELLING a private business concern what it can, or cannot, do?
Lydia Leftcoast
(48,219 posts)It's a pretty easy choice. Governments make laws. Companies are supposed to obey them. What's so hard about that?
1StrongBlackMan
(31,849 posts)Getting government to make the laws. In case you forgot ... Presidents don't make laws; they only sign (or veto) them.
marble falls
(64,371 posts)office and the FBI(for example) is part of the executive branch. President propose laws or directions and Congress acts on this one way or another.
Lydia Leftcoast
(48,219 posts)ASKING the insurance companies which laws they are willing to obey.
Having companies help write the laws that will regulate them is the essence of corruption.
Everyone on DU raised a stink when Cheney met with the oil companies behind closed doors, and rightly so.
So why was it OK for Obama to meet with the equally greedy and corrupt insurance companies behind closed doors? He did it before even the broad outlines of the ACA had been released.
Why was it OK to take the weakest possible bargaining position and START by offering what he thought the Republicans might accept? If he had started with single-payer, we might have ended up with a public option. Instead, he dropped both strong positions in favor of Romneycare, and the Republicanites still didn't vote for it.
A president with guts would have gone on TV FIRST and said to the American people,
"I am going to propose a single-payer system to Congress. It will have five main points: 1) Every legal resident of the U.S. will automatically be covered from birth, 2) There will be no deductibles (although there may be modest co-pays), 3) It will be financed by....(there are many possible alternatives, so I'm not naming one here), 4) Doctors and hospitals will still be in private practice, and you will be able to choose any licensed medical practitioner you please, 5) Visitors to the U.S. and illegal immigrants will be provided with care only for life-threatening emergencies and then sent to their home countries for further treatment. They will pay full price for non-emergency care.
"We can have this, just like Canada, the Western European countries, and most of the East Asian countries, if Congress will approve it. The insurance companies will sponsor media campaigns full of horror stories from supermarket tabloids or outright lies. They will try to bribe members of Congress to vote against it. If you want this passed, you need to call or write your House and Senate representatives and tell them that you want America to have not only the best but the most accessible health care in the world."
Then he would have rounded up the Democratic Congresscritters and told them to go to their home districts and reiterate the five points to their constituents in all public appearances. Congresscritters who refused (the Max Baucus types) would be told that the national party would fund a primary challenger who would accuse them of not caring about the health of the American people.
That's what a real leader would have done, not consult an industry about which laws they were willing to obey and make it hard for the public to find out what was in the ACA.
I had to Google like crazy to find an executive summary, and there was none on any government website. I finally found a summary on the website of the Kaiser Family Foundation. That's just wrong: trying to pass a piece of legislation that will affect everybody but leave the average American in the dark about what it contains.
That lack of transparency had three negative effects: 1) It allowed the right-wing to have a field day with horror stories from British and Canadian tabloids, even though the systems of the two countries are different from each other and neither is like the ACA, 2) People who were FOR health care reform THOUGHT that Obama was working on single payer. I heard this again and again, and having read the Kaiser summary, I had to correct them. 3) Since people had no idea what was in the bill, they were not motivated to lobby their Congresscritters.
Our only hope is that the states are able to put together single-payer plans on their own. I will be eligible for Medicare in a couple of years, so even Minnesota's strong effort will be too late for me, but I hope that future Americans, unlike me, won't have to go without medical care because their insurance premiums take up too much of their income.
truedelphi
(32,324 posts)Statements. But for some reason, (or lack thereof) the usual crowd from the BOG cannot understand the meanings that are being explained.
1StrongBlackMan
(31,849 posts)Anyone/everyone that took and passed an 8th grade Civics course should have a problem with that nonsense ... usual crowd from the BOG, or otherwise.
truedelphi
(32,324 posts)is how Obama went around all summer of 2009, telling one and all that he could not participate in the situation of using abully pulpit for anything related to the drfting of an insurance piece of legislation.
Then we come to find out that Rahm Emanuel and Liz Fowler were busy that same summer, initially using rooms in the "WH Basement" and then when activists started demanding to see the logs of whomever it was that Emanuel and Fowler were consorting with, then the meetings with the insurance CEO's began to take place some blocks away from the WH.
Together those two drafted a piece of legislation that was over 2,000 pages long, and basically written by the Industry. It was filled with give aways to the Big Insurers and mandates that will add immensely to the Big Insurers' profits, without many regulations in terms of price containment, or even ways for individuals to appeal the devious methods that Big Insurers utilize to avoid handling payments to the insured.
So there are several things going on here:
One DUPLICITY A President claims the following: 'Public option is but one tool in an entire tool box of options that Congress can employ. But since I am the President, and I am part of the Executive Branch of the US government, the separation of the three branches of government means I must bow out of the discussion until Congress has put its finishing touches on the piece of legislation that they re putting together.' (Obama's Answer given to Univ of Co student, Boulder Co, mid Aug 2009) But meanwhile his chief of staff is drafting the legislation with Liz Fowler and drafting it according to the whims and desires of the Big CEO's at Big Insurers.
Two: The wholesale deliberate evading and ignoring of what needed to be done. On this very board, I witness person after person lamenting Reagan.
But Obama is Reagan on steroids. We have gone from a nation where 9 cents out of every dollar of profit goes directly into the coffers of big banks, (circa the 1980's) to a nation where 49 cents out of every dollar of profit that is generated goes to the banks. All due to Obama appointments.
Perhaps if Obama had FDR as a template for his Administration and not Mr Reagan, (who let's face it, he praised and praised and praised in his autobiography), then we would still have a vibrant middle class. Instead, many thinking people realize we have been sold out.
1StrongBlackMan
(31,849 posts)Lydia Leftcoast
(48,219 posts)That is exactly the kind of thing that I was referring to in my criticisms of the ACA.
At the end of Bush's Reign of Error, people were hungry for some real reform...of a lot of things, not just health care.
But the powers-that-be, including a lot of the Democratic leadership, didn't want real reform, because they were doing just fine, thanks, so they found a young candidate with a lot of personal charisma who could talk a good game and play a populist on TV.
A lot of people who were too young to remember the Eugene McCarthy/George McGovern/Robert Kennedy era or who had never worked on the Dean or Kucinich campaigns were fooled.
I was always skeptical, and my skepticism was justified early on in Obama's first term. (Please note that this does not mean that I supported Hillary Clinton in the primaries. I voted Unaffiliated in my precinct caucus. I KNEW that Hillary Clinton is a corporatist through and through, but I would have voted for her over McCain any day.)
Cha
(309,260 posts)Will Pitt and his stupid anger issues which need management and is not the gift he pushes.


uppityperson
(115,920 posts)Cope with TOS.
Response to uppityperson (Reply #35)
Post removed
Response to uppityperson (Reply #35)
Name removed Message auto-removed
treestar
(82,383 posts)Did he specifically promise you this medication?
WilliamPitt
(58,179 posts)So, yeah.
Buck stops.
bluestate10
(10,942 posts)implement what was passed. BTW, on a personal note, I live in the same state that you live in or lived in. I think your claim is BS. I am in a plan that has mostly old and very ill people, I am in the minority as a younger healthier person. I watch those people filling prescriptions, I watch them going in to the examination room, NONE complain about being bankrupted to pay for medicine and as far as I know, none insist on a particular medication when their doctor offers effective alternatives.
MADem
(135,425 posts)for.
Move over the border to VT, see if you can get a better deal there....of course, they've got taxes too, pretty robust ones.
I think your anger is misplaced and I agree with those who said you should have checked the formulary first. Since you didn't do that, you need to work on appealing the decision, working directly with the pharmaceutical company that manufactures the drug, seeing if you can't get samples from a physician, or finding an alternative med.
Or move to VT.
But coming on DU and getting all dramatic and pouty? It's an old act, Will--it's immature and it's not getting that "Ooooh....ahhhhhhhhhh" reaction anymore. No, the ACA is not perfect but YOU didn't do your due diligence, either. And calling the POTUS childish names isn't going to fix your situation, it just makes you look like a petulant jerk.
brush
(59,431 posts)Get off it and get over yourself.
And btw, I hope your wife gets her meds and gets well.
one_voice
(20,043 posts)some people can do/say whatever they want with no repercussions.
That's something I'd expect to see at the cave, freeperville, etc. Not here.
I disagree with much of what the president has done/hasn't done, but damn.
I think Single payer/universal health care is what we should have gotten.
Standards only apply to some and more to others.
Autumn
(47,627 posts)one_voice
(20,043 posts)I got the same message you did.
The Straight Story
(48,121 posts)On Tue Mar 18, 2014, 05:09 PM an alert was sent on the following post:
Fuck you, Mr. President, you piece of shit used-car salesman. From my heart and soul, fuck you.
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686242
REASON FOR ALERT
This post is disruptive, hurtful, rude, insensitive, over-the-top, or otherwise inappropriate.
ALERTER'S COMMENTS
It seems there are better ways of expressing anger than this over the top one.
You served on a randomly-selected Jury of DU members which reviewed this post. The review was completed at Tue Mar 18, 2014, 05:15 PM, and the Jury voted 3-3 to LEAVE IT.
Juror #1 voted to LEAVE IT ALONE
Explanation: No explanation given
Juror #2 voted to HIDE IT
Explanation: No explanation given
Juror #3 voted to LEAVE IT ALONE
Explanation: No explanation given
Juror #4 voted to HIDE IT
Explanation: No explanation given
Juror #5 voted to LEAVE IT ALONE
Explanation: This alert is on the wrong post. Should be on the OP by WilliamPitt. This post by one_voice is pointing out the verbatum comment in Pitt's OP. It's obvious one_voice is dubious to this comment by WilliamPitt since the forehead slap emoticon is used. Alerter needs to re-read for comprehension.
Juror #6 voted to HIDE IT
Explanation: No explanation given
The Straight Story
(48,121 posts)I don't think the alerter thought it through very well ![]()
uppityperson
(115,920 posts)And I agree with what you write too.
Cha
(309,260 posts)Last edited Tue Mar 18, 2014, 11:14 PM - Edit history (1)
but, he finally got locked out of his own stupidass thread..
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686372
Edit: clarity.
alcibiades_mystery
(36,437 posts)Ouch.
Number23
(24,544 posts)This whole thread is just about one of the most cringe inducing, moronic things I've ever seen here. The OP needs to go sit his ass down somewhere.
It has never, EVER dawned on me to criticize a president because an insurance company didn't cover something I thought it should cover. And that includes every president (Repub or Dem) that have been in office since I got my first insurance plan.
Cha
(309,260 posts)one knows with Obama Hate comes many Recs.
It's too bad about the Med crisis with his wife in the state of New Hampshire but JHC .. don't compound it by taking it with a venomous attack on the wrong person.. even if that person is his favorite whipping post.
Whisp
(24,096 posts)A randomly-selected Jury of DU members completed their review of this alert at Tue Mar 18, 2014, 03:42 PM, and voted 3-3 to LEAVE IT ALONE.
Juror #1 voted to HIDE IT
Explanation: I sympathize with the poster's wife's medical situation; and if he'd even said 'fuck you Mr President for caving in' I would have voted to leave. But calling him a 'piece of shit used car salesman' is a step too far, and plays into the hands of the anti-healthcare Right.
Juror #2 voted to LEAVE IT ALONE
Explanation: So because "many others are finding that ACA is a blessing," those who find problems should just shut up? I would never have used the words that this person used to describe the president, however, the president can take care of himself. If this poster had directed those words at a DUer I would vote to hide.
Juror #3 voted to HIDE IT
Explanation: No explanation given
Juror #4 voted to LEAVE IT ALONE
Explanation: This is a long term poster. He is understandably upset by reality and angry, like many Progressives that the ACA was not enough, not sufficient, but was better than nothing. His outrage is understandable, a little over the top calling the President a used car salesman, but does not warrant disappearing the message.
Juror #5 voted to HIDE IT
Explanation: poster may be upset but this is over the top
Juror #6 voted to LEAVE IT ALONE
Explanation: I don't blame the poster for railing at the insurance company and the president for producing an inadequate health care act that benefits the insurance companies.
uppityperson
(115,920 posts)Cha
(309,260 posts)lostincalifornia
(3,639 posts)for certain now, is the standards are who happens to be on the jury, and it can vary from jury to jury
We can all understand the emotion involved however.
Cha
(309,260 posts)for will pitt to get his pos rage on.
Oilwellian
(12,647 posts)I suspect if it were your spouse's life at stake, you would be lashing out as well. It IS Obamacare that is the cause of Will and his wife's problem.
I find your comments cold and heartless considering the circumstance they now find themselves in. It's not ALWAYS right to defend fucking Obama.
Cha
(309,260 posts)insults in a prepubescent hissyfit that only got him locked out of his own thread.
mythology
(9,527 posts)It's poorly aimed and generally doesn't actually convince other people to listen to you. In my experience acting in anger and frustration is worse than stopping, calming down and then looking at a situation rationally and finding the best solution for the situation you're in.
Plus, there's information in this thread that could prove useful, but if he's too angry to hear it, then that won't help his situation.
And from the information given, I don't see how you can say this is the fault of the ACA. There's simply not enough information here to state that conclusively. For example, what specifically are his other insurance options in his state? And no, saying that somebody else told him not to bother isn't actually looking at options. Are there programs that can help pay for the drug regimen? Alternative treatment options? How specifically did the ACA cause this? If it's true that the plan is a grandfathered plan, then why wasn't the drug denied previously? Without knowing far more information that is presented, I can't say whether the ACA is part of the problem in this situation or if it's not.
But given how many times examples of how the ACA was causing somebody's insurance to go up, or get canceled have turned out to be inaccurate, I'm generally fairly cautious about believing such claims.
AnalystInParadise
(1,832 posts)of you to bash a guy that loves his wife and is angry. Typical.
Whisp
(24,096 posts)which could have been a positive learning to get advice and help from the many knowledgeable people here on the subject, but instead used the opportunity as a toilet to shit in.
AnalystInParadise
(1,832 posts)We don't see eye to eye on anything. BUT his wife is suffering, so I will exercise my humanity and not go to DEFCON 1 when he blows off some steam. If only other so called progressives showed the same humanity and humility. Instead some people want to settle scores and throw feces on a guy that is hurting that lost his cool. Give me a break.
Whisp
(24,096 posts)for reasons that I can only guess at.
AnalystInParadise
(1,832 posts)REAL PROOF of exaggeration, not anecdotal BS like so many around here treat as proof. I will gladly retract my support. Until then I see nothing wrong with a guy with a suffering wife venting his spleen.
brush
(59,431 posts)He seems to look for any reason to blast the President — obviously an Obama hater.
AnalystInParadise
(1,832 posts)has no bearing on today.......
brush
(59,431 posts)of behavior — anger management issues.
dilby
(2,273 posts)I am terrified of losing my insurance through my employer because I do have pre-existing conditions and if I have to go onto the ACA there is a good chance I will be in the same boat. The worst part is because this has become law and all Americans are required to have insurance there is no way to reverse this and move to a single payer option. The people once again get screwed while Insurance Corporations laugh all the way to the bank.
WilliamPitt
(58,179 posts)Tie a pork chop around your neck if you jump in; maybe it'll be over quicker.
![]()
NightWatcher
(39,360 posts)I'm in a similar boat, sick and uninsured (waiting on Medicare). What we should have got was Socialized Single Payer EUROPEAN Styled healthcare (note I didn't say insurance).
Sick and broke sux
obliviously
(1,635 posts)It is in the fine print
Lex
(34,108 posts)Sometimes that actually works.
lostincalifornia
(3,639 posts)requires this medicine and not and alternative, that usually does it.
A generic medicine did NOT work for me, but the brand name did. My Doctor authorized it, and it was covered. It did cost me slightly more though.
Hekate
(97,014 posts)... because that is the hoop I have to jump through. Otherwise the Rx company sends me the cheap generic with no notice -- and it makes me really sick. I give the letter to my doctor, he adds what he's required to add, and it gets faxed from his office.
Every year.
bvar22
(39,909 posts)Getting these parasites (For Profit Health Insurance Industry) to actually deliver quality health care is going to be the hard part.
As far as I can tell, The Affordable care Act provides NO Watch Dog Agency to hole the vultures accountable,
or no streamlined service to handle and expedite complaints.
It looks like we are still on our own if we feel we are treated unfairly.
We have to get a lawyer and file suit against these Mega Monsters and endure the years of financial hardship and distress necessary to reach a solution.
Sorry to hear about your problems,
and I sincerely hope you can find the needed medicines at an affordable price.
Bill Moyers
Republicans have now lost three successive elections to control the Senate and they’ve lost the last two presidential elections. Nonetheless, they fought tooth and nail to kill President Obama’s health care initiative. They lost that fight, but with the corporate wing of Democrats, they managed to bend it toward private interests.
So we should be clear on this, Obamacare, as it’s known, is deeply flawed. Big subsidies to the health insurance industry. A bonanza for lobbyists. No public option. And as The New York Times reported this week, “Millions of Poor Are Left Uncovered by Health Law.” Largely because states controlled by Republicans refuse to expand Medicaid.
http://billmoyers.com/segment/bill-moyers-essay-shutdown-showdown/
Health Insurance =/= Health Care
Aerows
(39,961 posts)Of course it doesn't. The main priority is to shield insurance companies and increase their profits. That somebody gets health care is a secondary consideration.
Hoyt
(54,770 posts)As bad as insurance companies are, they seldom deny mainstream meds unless it is to switch to an equivalent alternative. I'd check with state insurance commissioner if they are denying a whole class of meds.
Lex
(34,108 posts)which isn't the best plan in the world so I wonder if an appeal can work in Will's wife's case.
Hoyt
(54,770 posts)Doctor_J
(36,392 posts)The doctors prescribe medicine. The insurance company pays for it. Two steps, not one or two or five appeals, requiring the patient to act as physician, pharmacist AND lawyer.
My head hurts.
Lex
(34,108 posts)theboss
(10,491 posts)Insurance companies often limit a class of meds to one or two choices. It's frustrating, but it's been a part of health care for a while now.
Frankly, this was a lot easier when your choices were "Penicillin" or "an infection that will kill you by Tuesday."
bluestate10
(10,942 posts)although effective cause undesirable side effects, but resolving that type of problem is between the patient and doctor - the President and the ACA has nothing to do with that.
MADem
(135,425 posts)I think there's more here than meets the eye. The doctor may have indicated that an alternative medication would be just as efficacious.
Hoyt
(54,770 posts)when close alternatives are available.
MADem
(135,425 posts)The patient is allergic to an additive in the alternative; the alternative doesn't work as well on the patient, whatever....but if the doctor doesn't agree on the medical necessity, they won't go to bat just because a patient "likes" what they are on and doesn't want to switch to something new.
No formularies are more onerous than military medical ones--even for active duty people. The doctors generally will not go to bat to get a patient a med that is off the formulary without first trying the one(s) on it. But if it's obvious that the stuff ain't working, they WILL fold if the doctor insists. It's a pain in the ass but it can be done.
People who think single payer would "solve" this problem need to think again. What single payer is about is a minimum standard for ALL, not "every little optional or high end drug you want or need, when you want or need them."
The UK National Health doesn't hand out designer drugs or the high-end stuff as a first resort, either. Nor do they authorize cutting edge surgeries very easily, either. You have to "go private" for that. In fact there are parents who save/hold fundraisers to raise 40K pounds for specialty operations for children with cerebral palsy to be done in USA because they are not covered in the UK as a rule, and the few that are covered use an older system with a longer recovery time.
Hoyt
(54,770 posts)A couple of years ago, I was "forced" into Kaiser Permante and it didn't cover some of my meds. I griped, but eventually found their covered alternatives were fine.
No country can afford a wide open single payer system, and I'm fine with that. Heck, even Medicare has some large coverage gaps.
1000words
(7,051 posts)Do the math.
Some folks will tell you to be thankful for the crumbs. Fuck them, too.
bluestate10
(10,942 posts)wrong or are voted out of office. Neither of those outcomes come about by calling President Obama names.
1000words
(7,051 posts)Review my last sentence, again.
bluestate10
(10,942 posts)Reality is what it is. We won't get Single Payer until republicans have been routed. That is a fact that spinning fantasy doesn't change.
sendero
(28,552 posts)... we will not get single payer until there is a champion fighting for it. Obama is a champion of mediocrity and infinitesimal improvements. So there is that.
bvar22
(39,909 posts)It was the "Centrist" Democrats.
djean111
(14,255 posts)Centrist Democrats are pretty much Republicans. Non-centrist Democrats are jeered at and undermined.
The democratic party is run by the Third Way now.
Obama is a centrist. I have no reason to believe he would champion single payer if all of congress was Democrat.
TBF
(35,069 posts)there is no reason on this earth that we have to subject health care, water, shelter, education, etc to a for-profit system. We are being strung up by a bunch of billionaires who enjoy hoarding their wealth. The fucking system needs to go. We all know who the president works for (and so does he - and my guess is he doesn't want to end up like Kennedy so he is playing their game).
I don't know what else to say. We need more people as angry as you. But we need to be angry at the right thing & fix it. And we need to remember there are many more of us than there are of them.
And, no, it ain't gonna be easy.
PowerToThePeople
(9,610 posts)I was going to comment earlier on the banker jumper thread that they were just preempting the guillotine parade by jumping.
I understand the anger against the liar, he who said he had our backs but turned out not to.
Capitalism and the profit motive IS the real underlying problem here. It is the "root of all evil." Nothing will change for long while that system is still in place.
Lex
(34,108 posts)If you are taking medication for a chronic condition or something that has a high retail price, you may want to ask whether your plan maintains a separate list of specialty pharmaceuticals that are covered. You should keep in mind that the formularies are constantly in flux, and right now more than usual. For some plans on the exchange, the drug formularies are a work in progress as medical and patient advocacy groups continue to press insurers to add certain medications they think are important to cover.
bravenak
(34,648 posts)I sympathize but fuck that piece of shit nonsense. A write who can't come up with a better turn of phrase?
I never even called bush a piece of shit. And he was.
tridim
(45,358 posts)tridim
(45,358 posts)Sad.
zeemike
(18,998 posts)Sad.
tridim
(45,358 posts)zeemike
(18,998 posts)tridim
(45,358 posts)Congrats.
zeemike
(18,998 posts)And I am sure you will never look in it.
bravenak
(34,648 posts)Last edited Tue Mar 18, 2014, 09:01 PM - Edit history (1)
I hope he was hacked. We democrats are supposed to be above the juvenile name calling and be proactive with finding solutions. We can solve this problem if we work together. We all want single payer. I hope he contacts the drug company and asks the for the pills. They will often give them to you free if you cant afford them and it is good press for them. It worked for my neighbor downstairs. She and her doctor called them up and asked for them and they said sure. She has them now.
On Edit: my mistake. Name calling is apparently fine here. I will know better from now on not to mention it.
CJCRANE
(18,184 posts)There seems to be some slight confusion in the details, but obviously it shouldn't be this complex.
I hope he explores all the options and we get a happier update in the near future!
bravenak
(34,648 posts)Once he is a bit more calm perhaps he can post a thread asking for advice. If he gives the name of the drug and the manufacturer we can help him together to petition the for the drug he needs. Maybe together? I think we can solve this problem with out any further namecalling.
Wait Wut
(8,492 posts)Maybe you could send him a message with your suggestion. He's had a post hidden in this thread, so he can't reply here.
bravenak
(34,648 posts)I will try it in a bit. ![]()
Didn't know about the hidden post. We need to help him.
Cha
(309,260 posts)bravenak
(34,648 posts)No need for him to suffer in anger if he can be helped. He can go back to hating Obama right after he gets his (wife's)medication. I'm sure he has a whole slew of other complaints. I counld do without all the pieces of shit shit. I expect better from a literary master of his stature. My dissappointment with his verbiage is profound, indeed it is.
Cha
(309,260 posts)"Or...you can carry on without insurance, never getting to see a doctor, and die from the high blood pressure you didn't know you had.
I have been denied insurance for over 12 years. Scratch that...I was offered a 'plan' for $1200/mo that included a rider that excluded coverage for pretty much everything except falling out of my car. I now have a plan for $75/mo that doesn't exclude a damned thing and also covers meds for 50% of cost. Granted, it's been so long since I've been able to see a doctor that I'm absolutely terrified to go, now. But, I will...eventually. And, I will be grateful that I have insurance that will cover any catastrophic issues that may come up.
What Will is going through is tough, but he's received some helpful advice that he doesn't seem to want. I guess it's easier to be angry than actually fight. A lot of people are seeing real benefits from the ACA. Like everything else, this will be improved over time."
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686725
Bolding mine.
bravenak
(34,648 posts)I would like the piece of shit comment to be deleted. It is so depressing to hear democrats call democrats piece of shit right before the mid terms, or at all really. On DU, we can just say this about democrats? When did this start being okay? Is it only ok to call Obama a piece of shit? Or can we call any elected democrat a piece of shit on here? I would think that would be depressing for turnout in the midterms, and i assume we might, maybe, WANT, to win? Any nonmember curious about democrats in the mid terms might be very turned off thinking that democrats consider their own president a piece of shit. Or am i crazy? Dont we want to draw more curious left leaning people to our party? Not scare them away?
Cha
(309,260 posts)gobsmacked in the face. ![]()
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686372
Motown_Johnny
(22,308 posts)It is still possible for you to change your coverage so that the medication your wife needs can be covered starting April 1st.
WilliamPitt
(58,179 posts)Options:
1. Anthem BlueCross BlueShield
...and six days of rain.
sheshe2
(91,012 posts)bluestate10
(10,942 posts)why don't you cross the border into Massachusetts or Vermont and join better plans. Massachusetts is the best choice given the variety of plans available. I apologize, I thought that you lived in my state, you instead live in the currently second most backward New England state (next to Maine). The problem is your state, New Hampshire hadn't expanded Medicaid as of two months ago, even with Democrats leading the state.
Motown_Johnny
(22,308 posts)and blaming President Obama makes no sense at all. Most of us have a wide variety of choices.
Second, speak with a navigator just to make sure that BC isn't screwing you and that there is no better plan available.
Third, contact the manufacturer of the medication. Most companies have plans to help people afford the medicine they need.
Forth, look into a supplemental prescription insurance. I had some company send me cards for one last week. I gave them to a friend who has health issues in the hope that she can enroll with that company. I can look into it if you have issues finding something.
I wish you and your wife the best. I have to believe that there is an answer out there for you and I hope you find it.
Purrfessor
(1,190 posts)My wife's doctor prescribed a new medication. The first eScripts rep I spoke to said it was not covered. I called a second time and was told by a different rep it was not covered by eScripts but was covered by their specialty pharmacy, Accredo, which dispenses these newer, specialty drugs. The rep connected me to Accredo. I provided them the requested info from our end. They contacted the doctor and within 10 days we received the prescription. It was covered. I just had to speak to the right person in order to navigate the maze. Your situation may be different but you should inquire further. If eScripts is your mail order pharmacy, call and ask them about Accredo and if the drug is available via that route.
JoePhilly
(27,787 posts)Particularly ... this section...
http://www.nationalmssociety.org/Resources-Support/Insurance-and-Financial-Information/Health-Insurance/Appeals
Looks like hey provide materials to help you and your doctor appeal such decisions.
steve2470
(37,468 posts)MS One to One, www.msonetoone.com or call
1-855-MSOne2One (1-855-676-6326)
This was for Aubagio. The other MS drugs, I'm guessing, may have similar pages.
DebJ
(7,699 posts)tridim
(45,358 posts)1000words
(7,051 posts)msongs
(70,994 posts)better
treestar
(82,383 posts)And the entire ACA would be just fine, it if met one person's specific needs only? You'd throw out coverage of everyone else over this?
And why not fuck Congress and Joe Lieberman? What did you think the president was, a magician who could just make them pass a good single payer system? I wish we had that too, and no doubt so does Obama. But not enough of our fellow citizens do.
WilliamPitt
(58,179 posts)They are providing general coverage, and then denying coverage for specific medications.
Which makes the general coverage useless. My wife can go get a free scan that shows how fast her disease is ravaging her, because she doesn't have the medication she needs.
Shell game, tree.
I have heard of other cases similar to yours. Granted they are only anecdotal but they come from an internet community of those who have NF1.
lostincalifornia
(3,639 posts)to investigate the viable pharmacy's in Canada
bluestate10
(10,942 posts)implementation of the ACA? Were there restrictions on the use volume? Unfortunately the ACA didn't fix all problems - the President has to implement the law and has only limited levers that he can use during implementation, and when he uses one of those levers the right goes bullshit.
Why do you think the President can and/or should tunnel down to a plan prescription policy and override that policy? The right would be calling him a love child of Stalin and Hitler if the President corrected a bad local plan.
You live in a state that doesn't offer a good choice of plans. That sucks for you and is wrong, but understand that isn't the fault of the President.
pnwmom
(109,801 posts)And with regard to medications, formularies have to include choices from every class of medications.
You need to check all the formularies of insurers available to you, both on and off the exchange. Your agent friend is wrong about that being a waste of time. He's either being lazy or he has a vested interest in your staying with whatever plan he found for you. Or both.
theboss
(10,491 posts)Is the problem this one specific medicine is not covered?
This is a common problem - going from one plan to another and having a drug fall off the formulary.
Sometimes, you can get it added. Sometimes, you can find another drug.
Of course, you provided no info here.
dembotoz
(16,922 posts)when you give a weasel
the chance to be a weasel
it will be a weasel
because it is a weasel
there should have been a button labeled
who does this fuck
on the information page for the plans
Lydia Leftcoast
(48,219 posts)but do you have contacts in Canada who could write a prescription that you could buy for a reasonable price?
Elderly snowbirds from Minnesota who winter in Texas or Arizona buy their meds in Mexico.
lostincalifornia
(3,639 posts)Canada through mail order. People do that all the time. You need to make sure it is an accredited pharmacy and research it out, but that should work
MADem
(135,425 posts)If he gets to Canada by lunchtime he can be home for dinner.
Aerows
(39,961 posts)is like 1/4 the cost of a prescription in the US. Why people don't see this as a problem, I will never know. Why are there no regulations to prevent price-gouging?
If something costs 1/4 of the price in another country, somebody is profiting handsomely and basically robbing the public.
lostincalifornia
(3,639 posts)which is why ours are more expensive.
Whether that has any validity or not I do not know, but one thing is certain, Congress had opportunities equalize the issue, and does everything to subvert it
Aerows
(39,961 posts)Nobody sells anything unless they profit from it. Drug companies wouldn't sell it in other countries if they didn't make a profit from it. They just have free rein in the US to charge whatever they think they can get away with, even if it comes down to life or death for their fellow human beings.
lostincalifornia
(3,639 posts)Aerows
(39,961 posts)Congress couldn't operate a bake sale without screwing it up, never mind managing a nation's legislature. There are only a handful of them that actually give a damn about the American people.
(Oh, and your post is 666 ... spooky) ![]()
![]()
lostincalifornia
(3,639 posts)Aerows
(39,961 posts)I didn't mean anything by it, I just noted the number. ![]()
lostincalifornia
(3,639 posts)Aerows
(39,961 posts)It was a playful post.
lostincalifornia
(3,639 posts)Aerows
(39,961 posts)I've probably angered an entire legion of Obama fans, but I will relate my story, and join with the other voices that demand better than we have health care.
lostincalifornia
(3,639 posts)Aerows
(39,961 posts)is a thoroughly corrupt system where lobbyists write the laws and Congress members sign them in exchange for campaign donations.
That's the main problem, and it doesn't just happen in the health care industry. I wish I had a solution to the problem, but I don't. The system will only change when it buckles under it's own weight.
Common Sense Party
(14,139 posts)If so, it's surprising that this wasn't known BEFORE the ACA was passed and rolled out.
bluestate10
(10,942 posts)reddest New England state. Even though New Hampshire is led by Democrats, as of two months ago, it hadn't done Medicaid expansion. I live in Massachusetts, I have yet to see patients get denied needed medication or have problems paying for it. The ACA was modeled after the Massachusetts plan.
Let me get something straight. Don't call the Massachusetts system RomneyCare. The Democratic Legislature in Massachusetts had to repeatedly override Romney vetoes to get the plan we have. If Romney had his way, Massachusetts residents would have had a fucking barbaric healthcare system.
MADem
(135,425 posts)are very satisfied.
It's fun to call it "Romneycare" for one reason, though--to fuck with Romney! He used to get so MAD when people would say it, so it's a great "Nanny nanny boo boo"--hell, this thread is all about behaving in an immature fashion, after all....
![]()
dionysus
(26,467 posts)Mr.Bill
(24,906 posts)to cover the stiff drink.
dionysus
(26,467 posts)Bluenorthwest
(45,319 posts)what. There is nothing so enraging as seeing a loved on suffer needlessly. I am very sorry she's having to endure this. It is unconscionable.
Auggie
(32,172 posts)No way
dilby
(2,273 posts)When I saw the ACA I immediately saw a system where the people would be ripped off by Insurance Corporations. Single Payer was the only solution because now every American can have health insurance but it does not mean they can have healthcare.
CJCRANE
(18,184 posts)Channel that anger and get the DU crowd into action!
Response to WilliamPitt (Original post)
nadinbrzezinski This message was self-deleted by its author.
nadinbrzezinski
(154,021 posts)Still services should be able to help. That is what they do.
nadinbrzezinski
(154,021 posts)I will self delete cause it matters not, and gave him the exact same advise on the FB. Coming from me it means bird droppings or something like that. He should include the insurance commissioner as well.
The only thing I will add to this, is that this is why we need single payer, period. I am not holding any hopes the present dysfunctional political system will give us results friendly to the people's needs. We need far more than people pissed off on website.
rudolph the red
(666 posts)nadinbrzezinski
(154,021 posts)That still applies.
It does not matter what state you live in. Never mind, that is less valuable than bird droppings since it is coming from me. I mean that.
rudolph the red
(666 posts)sorry, didn't mean to be negative, just wanted to be accurate.
Douglas Carpenter
(20,226 posts)the insurance companies. That is the simple reality our utterly corrupt and depraved political culture.
LiberalAndProud
(12,799 posts)The ACA has been a boon for some, and I'm genuinely glad for them.
So. Now you're faced with the question of paying for the medicine your wife needs or paying for your insurance. Would that be a fair assessment?
So. Let's celebrate our contribution toward reducing the deficit.
![]()
Obamacare falls far short of what it should have been. I guess the president is as good a receptacle for our disappointment as any. The legislation we ended up with probably has nothing to do with the debacle that was Mrs. Clinton's task force. Probably.
seveneyes
(4,631 posts)That made passing the bill before we could see what was in it a real problem. I am afraid there will be many more people in a similar situation before it gets any better.
cheapdate
(3,811 posts)The house and senate worked separately on different approaches to health care reform. The house debated several different approaches and approved of legislation that included a public option (which was the approach favored by the president). The senate advanced a bill out of the Finance Committee. This was the bill that eventaully became law.
I'm not going to recount the entire series of procedural steps that eventually led to passage of the senate bill. Suffice it to say that up until right near the end, the house continued to fight for its legislation and the senate continued to push for its bill to be adopted. With time running out, house leader Nancy Pelosi conceded and brought the senate replacement bill to the house floor for a final house vote.
The house approved of the senate changes and when asked by the press about the vote, Pelosi said with resignation and I'm sure no small amount of frustration that she hadn't read the bill. Her entire energy had been focused for more than a year on passing the house bill. She hadn't read the senate bill.
But by no means does that mean that no one read or understood the senate bill before it was passed. The "Baucus Bill" had been under consideration in the senate finance committee as early as 2007. The committee published an early draft of the bill in November 2008, just days after Barack Obama's election. By that time, the senate had been holding hearings on the bill for more than a year.
The bill would not be passed until after another year and half of hearings and debates. During that time, it was subjected to the most intense interest, scrutiny, and debate of any other single piece of legislation in my lifetime. The debates took place in Washington and around the entire country. The bill itself was publicly available for this entire time. Many people read and reviewed it.
Both the bills (the house and senate versions) were publicly available. Both bills were thoroughly reviewed and scored by the CBO. Both bills were thoroughly scrutinized and reviewed by numerous health policy institutions who published review papers, summaries, and guides for anyone who was interested. Private and professional groups with an interest reviewed the proposed legislation exhaustively. Anyone who was interested could review the bills. I did.
seveneyes
(4,631 posts)Should have been written in stone. Inexcusable.
cheapdate
(3,811 posts)any viable system will include cost controls. Even a not for profit public system will have cost controls. That's reality.
As it was, the health care reform law passed without a single vote to spare -- including all 58 Democrats and both independents (Lieberman and Sanders). Robert Byrd had to be wheeled onto the senate floor in his wheelchair to cast his late-night vote for cloture to move the bill for a full vote.
The Democrats had a 60-vote majority in the senate for only a window of time -- between the time when Sen. Al Franken was finally seated and the time when Scott Brown won the special election to replace Ed Kennedy.
It's easy to call the health care law "inexcusable" but it could have just as easily fell short by one or two votes and died -- just as the DREAM Act did.
We would have completely blown any opportunity to make any positive change. Insurance companies would be free to continue dropping policy holders when they get sick, denying coverage to the very people who needed it the most, etc. There's no telling when, if ever, there would be another opportunity. Certainly not now and not in the near future either.
It's easy to call it "inexcusable" when you're not the one counting votes in the senate and weighing chances for winning or losing while the window for action is closing.
I think the law does a lot of good and is a good start. The SCOTUS decision on Medicaid expansion was a big blow, but in the long run it may help to turn opinion in some red states where governors and legislatures have refused the expansion, so it too may wind up being a positive.
One day we may have a congress ready to work again to improve health care. Obviously, that means a Democratic congress because as long as the Republicans have any control at all it's not going to happen.
Vote for progressive Democrats.
Skip Intro
(19,768 posts)I'm sorry you and your family are among them.
ProSense
(116,464 posts)In fact, it's the OP's responsiblity to check to see if his insurance company covers his family's medications.
Drug formularies are not the President's decision, and existed before the ACA. They exist in Medicare Part D.
The one thing the ACA did do is introduce a new rule applicable to appeals.
The Affordable Care Act ensures your right to appeal health insurance plan decisions--to ask that your plan reconsider its decision to deny payment for a service or treatment. New rules that apply to health plans created after March 23, 2010 spell out how your plan must handle your appeal (usually called an “internal appeal”). If your plan still denies payment after considering your appeal, the law permits you to have an independent review organization decide whether to uphold or overturn the plan’s decision. This final check is often referred to as an “external review.”
http://www.hhs.gov/healthcare/rights/appeal/appealing-health-plan-decisions.html
Lex
(34,108 posts)But that wasn't going to pass at all.
Doctor_J
(36,392 posts)He lied about that in the campaign.
I'll take your word for it that you know what he personally wants in place as opposed to what could reasonably pass.
bvar22
(39,909 posts)but couldn't support it here because we would have to "build it from scratch",
and it would be easier to build upon our existing private system.
Now, "build it (Single Payer System) from scratch" is indeed a LIE.
There are TWO Pre-existing successful Single Payer Systems if the USA:
Medicare and the VA.
We could have expanded either one.
Skip Intro
(19,768 posts)Obama said, clearly, if you like your plan you can keep it. He said clearly if you like your doctor, you can keep your doctor. No if that, or unless this. In fact, he said period. Repeatedly. For months. And he knew it wasn't true. Those are and were lies. If you claim to others that something is true, and you know it to be false, you are lying. He said people's rates would go down, $2500 per year for the average family. Rates went up substantially, skyrocketing for many, making it unaffordable for some. He had to know that was a false claim too.
Millions of real people have been negatively affected by the ACA, after they were told, promised, lied-to, that they wouldn't be. They have every right to feel betrayed.
So trust is lost. Thing is, when you lose trust, thinking people won't believe anything else you have to say, either. Does anybody believe his assurances that the NSA isn't spying on the American people at large? I don't know anyone who takes him seriously on that. It is assumed he is lying at this point.
Btw, saying to people like Will, and as I believe you have said to me as well when I relayed a negative experience with Obmacare, that in essence, we shouldn't have believed the hype from Obama, and should have read the fine print, is a lowly tack to take after the fact.
ProSense
(116,464 posts)"Obama said, clearly, if you like your plan you can keep it. "
...the hell does that have to do with the OP?
Skip Intro
(19,768 posts)I don't think even you buy you at this point.
ProSense
(116,464 posts)It's fly paper for those who want to attack the President based on inaccurate information.
Skip Intro
(19,768 posts)Because spinners come along and do their best to obscure those facts, often by attacking the character of the messenger.
Rex
(65,616 posts)Have to agree with your assessment.
Demo_Chris
(6,234 posts)bluestate10
(10,942 posts)because my use rate goes outside a model. When rejected, I tell the Pharmacy to fill the prescription and I pay for 100% out of pocket. This happened before the ACA and hasn't changed.
There may be alternative medications for your wife that are less expensive, medical plans default to the least expensive medication that works. I don't know your wife's medical details, so I won't render an opinion, I just related my personal experience with medication.
Aerows
(39,961 posts)Why is it that a prescription for a common drug in the USA costs 4X more than it does in, say, Canada?
Do you happily pay 4X more for anything else besides a prescription and think you are getting a great deal?
Bernardo de La Paz
(53,951 posts)There is too much desire for all-or-nothing perfection.
I"m sorry about your wife's condition, but go ahead, take nothing or take the better deal you had before ACA.
dilby
(2,273 posts)So what you have insurance, doesn't mean anything if it does not cover the stuff that saves your life. So you can go get a checkup that is great and the doctor can tell you that you have high blood pressure but you still have to pay out of pocket for the medication.
...you can carry on without insurance, never getting to see a doctor, and die from the high blood pressure you didn't know you had.
I have been denied insurance for over 12 years. Scratch that...I was offered a 'plan' for $1200/mo that included a rider that excluded coverage for pretty much everything except falling out of my car. I now have a plan for $75/mo that doesn't exclude a damned thing and also covers meds for 50% of cost. Granted, it's been so long since I've been able to see a doctor that I'm absolutely terrified to go, now. But, I will...eventually. And, I will be grateful that I have insurance that will cover any catastrophic issues that may come up.
What Will is going through is tough, but he's received some helpful advice that he doesn't seem to want. I guess it's easier to be angry than actually fight. A lot of people are seeing real benefits from the ACA. Like everything else, this will be improved over time.
Number23
(24,544 posts)Bernardo de La Paz
(53,951 posts)Affordable is better than nothing, even if it is far from perfect. I doubt if anything better could be gotten through in this day and age. It will have to wait for another Democrat, who will push through a better system in a more receptive time and will probably be accused (with some truth) of also being a "used car salesman" because even that system will not be perfect.
dilby
(2,273 posts)A single payer option like Medicare with the ability to purchase private insurance if you wanted the Mercedes Benz version of healthcare would have been the solution. It would have covered everyone without them paying to make a private company richer and it would have silenced people who prefer their existing healthcare.
Lex
(34,108 posts)that wasn't going to have a snowball's chance in hell of passing. Not at this point.
dilby
(2,273 posts)We have a system that basically says you have to pay a healthcare tax to a private company that may or may not offer you services.
Bernardo de La Paz
(53,951 posts)... regardless of what Justice Roberts wrote in his opinion.
Lex
(34,108 posts)people get used to most everyone being covered, they are going to want more and the overall savings that single payer would bring.
jeff47
(26,549 posts)The ACA moves the battle to the states. It's much, much easier to pass single-payer or public options in blue states.
Those plans won't have the 20% profit, so they'll be cheaper, causing some to switch. Those plans won't result in a pile of dead bodies, causing more to switch for price. That gives a better risk pool, making the public plans even cheaper. Private insurance won't be able to compete.
With real-world examples in those states, it's going to be much, much easier to create such plans in purple states. Which will follow the same course.
All those examples will make the national battle much, much easier.
Bernardo de La Paz
(53,951 posts)truedelphi
(32,324 posts)maybe you'll "get it."
Health insurance is not health care. And unless you have decent insurance through your employer, or you are rich enough to have a premium policy, you will indeed find out that carrying around a bright and shiny plastic card that you pay X amount of each month for the privilege, is only something offering you the right to sit and listen to elevator music on the insurance appeals' line.
brush
(59,431 posts)If you have a health insurance plan you do not have to cough up out of your own pocket the thousands of dollars to get treatment in a hospital.
You have to know that paying the full bill for just a day or two or three in a hospital can break the average person.
With insurance you will pay a just percentage of it.
Bernardo de La Paz
(53,951 posts)Maybe you'll get that. At least they'll have some care even if it is not gold-plated US House of Representatives member care.
Duval
(4,280 posts)Response to WilliamPitt (Original post)
Name removed Message auto-removed
boston bean
(36,754 posts)Weren't you mandated prior to ACA to have health insurance?
Did your prior plan cover the medication?
I'm sorry your wife has been denied medicine she needs. That really sucks and should not be happening in a civilized society.
MADem
(135,425 posts)Duval
(4,280 posts)my husband, I would have felt not only anger, but fear. We are retired, and our secondary insurance is Blue Crap, Bull S&*t. They upped the price of meds we take as well as the percentage of our co-pay. I just hate it for you and your wife.![]()
![]()
![]()
lumpy
(13,704 posts)naturallyselected
(84 posts)Won some, lost some. It stinks, but I didn't expect this to change under the ACA. I have found it is sometimes worth the fight - I have unexpectedly won a couple of battles.
I came across this article from the Toronto Globe and Mail. A couple years old now; I don't know if the situation has improved.
Link:
http://www.theglobeandmail.com/news/national/time-to-lead/the-cost-of-drugs-breaking-the-bank-to-stay-alive/article4263623/?page=all
Clip -
Julie Easley had just graduated from the University of New Brunswick when she was diagnosed with Hodgkin's lymphoma. She was 23 and broke - with exactly $9 in her bank account.
Thankfully, in Canada, her medical care was free of charge - or so she thought.
In fact, while physician visits and in-hospital care like chemotherapy are covered by medicare, Ms. Easley soon learned that the essential medication she needed to take out-of-hospital was not.
End clip -
So single payer doesn't necessarily solve this problem. I don't know what percentage it is, but many in Canada buy private drug insurance for just this reason.
I'm sorry to hear this. As long as the pharmaceutical companies want the prices they do for some medications, we're stuck with these tragic occurrences.
kardonb
(777 posts)only illiterate people need to resort to foul language ! You should have informed yourself about medication coverage the Co. you signed up with provides . ts always cheap and easy to blame everyone else for your own mistakes . Grow Up .
meanit
(455 posts)if he checked the medication coverage prior to signing up? It's still not covered and it doesn't sound like any of the plans cover it, but he still has to have the insurance by law.
Hissyspit
(45,790 posts)You are complaining about a long-term poster's use of language, which has ALWAYS been allowed here in the interest of freedom of ideas, and you start your post with "fu?"
Right.
Agony
(2,605 posts)fuck this uncivilized bullshit and anybody who supports it. this is not complicated, end of story.
I have encountered this personally, sorry Will (and anybody else) that you are dealing with this. The same anger flows through me.
This is one of the reasons why _we_ are not exceptional.
steve2470
(37,468 posts)see my post at http://www.democraticunderground.com/10024685964#post164
pacalo
(24,741 posts)Prescriptions are expensive -- something lost on those who served as jurors on his hidden post.
Between my husband's very expensive medications & those for my son, we couldn't afford their monthly prescriptions without the help of our insurance coverage.
I would be as livid as Will if the same happened to us. I hope Will uses his anger to right this wrong.
Whisp
(24,096 posts)consistently overwrought hate and misdirected anger toward this administration under a whole lot of subjects.
pacalo
(24,741 posts)Considering all the roadblocks Obama has to contend with, I think he's among the top presidents in my lifetime. He's a victim of circumstances (the PTB) in many issues that cause arguments on DU.
However, Will has a right to be very upset about this issue.
brush
(59,431 posts)pacalo
(24,741 posts)And it's okay for a Democrat to have anger issues with the president; he's a public figure who makes decisions that impact our quality of life. Whenever I see a Democrat have anger issues with president, I understand that the president has harmed someone's interest on issues very important to them.
Whisp
(24,096 posts)That one has been banned a couple of times from DU but somehow manages to come back and start the road there again and again by not being able to control his anger.
Sorry, calling the President a piece of shit is Not acceptable. That is something some asshole teabagger would say in Congress or at a moron rally. It is Not acceptable here.
brush
(59,431 posts)And it even makes me wonder why this extreme anger is being openly voiced on DEMOCRATIC UNDERGROUND (THIS IS NOT FREE REPUBLIC AFTER ALL) towards a black president — who happens to be a DEMOCRAT.
COME ON, ALREADY!
He went waaaaaaay too far with his choice of words. And he's a writer no less. No excuse for calling the president a "piece of shit."
marble falls
(64,371 posts)blindersoff
(258 posts)I am on an MS injectable drug and when I changed insurance through my employer in November found out that my cost would go up almost $100/month (from $80 to 175). My insurance company advised me to call the Pharma company and ask them about copay assistance. It took about 3 weeks to get it all together, but my copay is now $10 per month. Just goes to show you how much the mark up is on these drugs. The caveat was that I could not be on Medicare or Medicaid in order to get this copay assistance. Good luck to you and your wife. Keep her from getting stressed out (and you too!)
tarheelsunc
(2,117 posts)Whether or not it covers specific treatments for specific conditions depends on 1) if the plan is required by law to carry that and 2) if the company chooses to add that coverage on their own. Like others have said, you should be able to get info on what's covered by the insurer and what's not before actually enrolling.
steve2470
(37,468 posts)which apparently is a commonly prescribed drug for MS. I looked it up on my website for my plan with Blue Cross Blue Shield of Florida at http://bit.ly/1gyyj5M (password required for a member).
It's not covered under my plan and I pay good money every month for my policy. Cost per month (if one had to have this per one's doctor) runs $4,868.41 per this site.
I guess all I'm trying to say is, you are not alone in your predicament. If I or my son were to be diagnosed with MS and require Aubagio, for instance, I would be in serious financial trouble.
![]()
Wait Wut
(8,492 posts)...without really being educated on the drug or the disease, the site looks like it has some options. I also researched a few other drugs and they all seem to have some type of solution to the (ridiculous) costs of the mediations.
https://www.aubagio.com/aubagio-copay?s_mcid=PSAOGO37
steve2470
(37,468 posts)I saw that page after I made my post. If I had to take that drug, I'd be beating down every door I could find to afford it. It's "retail price" is just unaffordable.
Wait Wut
(8,492 posts)...and not the President. Hell, I'm only half blaming the damned insurance companies for this. I am curious to know what they end up paying compared to what you or I would pay, though. I'm fairly certain they aren't shelling out 5 grand.
From what I've read here and a few other places, our friends in Canada are in the same boat with medications. Single payer doesn't seem to be a complete solution. So, we need to start going after the right companies for the right reasons.
Years ago, I remember this being a priority. I think we've become sidetracked with other issues and forgot that people can't afford to take their damned pills. Will has the opportunity to make this hot DU issue, but I think he needs to refocus his energy a bit. His anger has gotten the best of him, which I can somewhat understand, but it isn't going to change anything.
steve2470
(37,468 posts)Of course, big pharma has to make their enormous profits before they lose patent protection, and Wall Street usually loves the pharma companies for their profits.
Health care for all before profits, not the other way around.
Wait Wut
(8,492 posts)...what are we going to do about it? I have to admit, I was surprised to hear that Canada has the same issues. Can we put a target on big pharma and make it stick this time? I'm going to assume they're a little nervous with all that's going on in healthcare. Maybe now is the time to start pulling the curtain back and putting them back in the spotlight.
one_voice
(20,043 posts)Yes, yes, yes.
Pharmaceutical companies are horrible.
This is an old article, but it still applies.
According to one study, Americans paid an average of 54 percent more than Europeans for 25 commonly prescribed drugs. Some essential drugs are especially costly in the United States. A month's supply of Eldepryl, a Parkinson's disease medication from Somerset Labs Inc., costs about $28 in Italy, $48 in Austria and $240 in the United States.
*snip*
http://www.nytimes.com/1991/05/24/business/why-drugs-cost-more-in-us.html
another one http://www.cnn.com/2004/ALLPOLITICS/01/27/timep.drugs.tm/
I can't find a more recent article. The only thing that has changed is it's gotten worse, imo.
marble falls
(64,371 posts)Wait Wut
(8,492 posts)...when this was a hot issue here and everywhere else. We got sidetracked with the ACA. I think it's time we refocus.
Aerows
(39,961 posts)Here, they just charge whatever they think they can get for it. They might as well be holding people at the barrel of a gun because if it is a choice between life or death, most people will choose life until they drown in debt.
Wait Wut
(8,492 posts)It makes the US look like a country full of fools. I tried finding some politician or anyone, really, that seemed to have an interest in making changes and couldn't find a damned soul. This weekend I'm going to start sending out some emails to people I think may give a damn. If you have any suggestions of names to add to my list, I'd appreciate it. It probably won't do a damn bit of good, but we have to start somewhere.
I'm grateful that I can have insurance after 13 years. But, there are still too many people suffering because of the cost (and denial) of prescription medication. It's damned heartbreaking.
lostincalifornia
(3,639 posts)change insurers since this is before March 31. If they don't, then see what appeal process is available with the insurer.
Politicub
(12,309 posts)That's the first thing I look at when presented with health plan choices. My husband has several medical problems, and not all insurers cover his durable medical and medication needs. This is the reality in which we live.
I think this is an episode where you should look in a mirror and shake your fist. It's research you should have done, and blaming the President seems counterproductive.
But yes, fuck for-profit insurers. I'll join you in saying that.
The ACA needs a lot of fixes, but getting away from job lock just for health insurance is so important to many of us.
I'm really sorry to hear about your wife, and hope you are able to find a solution to getting the cost down for the medicine she needs.
On edit: did you try this?
https://www.healthcare.gov/what-if-i-want-to-change-marketplace-plans-after-i-enroll/
jamzrockz
(1,333 posts)about your situation, which insurance company, which drugs etc etc. Maybe someone around here with the knowledge could help you figure this out. ACA is not perfect but we have to chill down and work this out like adults.
spin
(17,493 posts)and progressive site such as DU so many are finding fault with the ACA.
I have long wished that our nation had a truly world class healthcare system and consequently that has been a main reason that I have voted for many Democrats over the years.
To me it is obvious that the supposedly most powerful and wealthy nation in the world should have a good healthcare system for all citizens. The one we had was at least twice as expensive as that in many nations and inferior to most.
So I celebrated Obama's election and hoped that those in the Democratically controlled Congress would look at all the other healthcare systems in the world and pick the best features of the best to create our own. I didn't expect it to be inexpensive but I did feel that a properly designed plan would save the average person a lot of money but deliver a higher level of care.
I'm not sure why we ended up with the plan we have but I have to admit that I was disappointed. Still I felt it might be a good first step and with some effort it might prove far better than what we had which would not be a major accomplishment.
Of course the Republicans, the party of "NO", oppose ObamaCare and are are trying to repeal it. Considering their opposition to any policies that Obama advocates this is not surprising. Most Americans wish to keep the ACA but many wish to improve it so it is far better and cheaper.
This thread greatly disturbs me. When a long term poster such as WilliamPitt finds serious fault with the ACA and many other posters here agree with him, I fear we have a serious problem. How can we rectify this and how do we win seats in the midterm election or put another Democrat in the White House after the next Presidential election if ObamaCare is widely unpopular even with progressive liberals?
I was hoping for something like Medicare for all. I currently am retired and on Medicare with an excellent Medicare Advantage Plan. While not cheap, I find it affordable.
Last year I had a fairly serious operation which required me to stay in cardiac intensive care overnight and also involved a lot of expensive tests and office visits prior to the procedure. My out of pocket expenses for all the office visits, the tests and the operation and overnight stay was $0.00.
I now understand that the costs of Medicare and Medicare Advantage Programs will likely rise significantly in the future to help finance the costs of the ACA. If so, and I have another major medical issue, I may end up with no funds and living on cat food. I guess if there are major changes to Medicare, I best hope that I have a major heart attack and die in my sleep. Admittedly I have lived a good life and currently am currently contributing little to our society or the wealth of the rich and powerful who run it. Since I am an unproductive citizen why should my government waste money on me while it can spend that money on a far more productive citizen. The fact that I served in the military during the Vietnam era and worked all my life and paid taxes is totally irrelevant.
Lars39
(26,351 posts)spin
(17,493 posts)I filled out all the paperwork twice over two years but was rejected because the VA felt I had too much money in my 401K. (I'm far from rich.) I also am only a Vietnam era vet and didn't serve in a war zone but was stationed stateside during my entire enlistment. (I have few war stories to tell my grandkids. I have tremendous respect for anyone who actually served in Vietnam. In my opinion they deserve VA care far more than I do.)
I have to admit that I somewhat disappointed as when I enlisted I seem to remember that I was promised lifetime healthcare. Perhaps I would have had this care had I signed up right after I left the service but I was always had a excellent healthcare plan through my employer for a very reasonable price.
I recently had a conversation with an employee of a local VA healthcare center. She told me to bring my DD Form 214 to the VA hospital and try applying again. I should take her advise and likely will if major changes occur to Medicare. Perhaps things have changed over the last five years.
Lars39
(26,351 posts)My brother was one, too.
Hoyt
(54,770 posts)are quite popular. Traditional Medicare without a supplemental policy has no out-of-pocket cap, and lacks the coordination of care that is so important nowadays. Traditional Medicare does not cover everything either, nor do health systems in many countries like Canada and Britain.
I think Obama got the best he could get as far ACA with the Republican opposition. Something had to pass, or we'd be stuck with the status quo for decades just like what happened when Hillarycare was defeated.
I'm not optimistic about midterms or 2016 or what will happen if Republicans take charge.
With this issue, I think some information is missing, but because OP had a post hidden, he can't respond.
spin
(17,493 posts)I was eligible for Medicare.
Medicare with the Medicare Advantage Plan I have is even better and while it is not cheap the cost is very reasonable. I've had excellent care with Medicare and my operation was preformed at a highly rated university hospital. I have no idea how much all the office visits, tests and the operation would have cost, but I'm sure they would have put a major strain on my assets.
I will agree that I have great hopes for the ACA and feel that eventually it will live up to its promise. Unfortunately that far less likely to occur if the Republicans win big in the midterms and the next Presidential election.
Skittles
(163,106 posts)yes indeed
Aerows
(39,961 posts)is that there are no price controls whatsoever on health care. Ask me about an $18,000 hospital bill that I walked into the emergency room for, walked out of it an hour later, and then got 4 shots that took five minutes a piece.
And of course, the health insurance company declined it. Homeowner's insurance declined it. Unless a deity comes down and declares that it is covered, you are denied.
Having insurance is great - unless you actually use it.
Health insurance has absolutely nothing to do with receiving health care. You basically pay into a system that might do something for you if it doesn't cost very much, but when it comes to catastrophe, you are on your own.
I can tell you stories about Worker's Compensation claims being denied because a procedure was $900. Apparently, getting a piece of metal embedded in your arm if you work as a mechanic is outside the realm of coverage, and "nobody could have foreseen that happening" despite paying a shit-ton in premiums for years with no claims.
truedelphi
(32,324 posts)Rahm Emanuel and Liz Fowler.
They spent the summer of 2009 meeting with insurance and pharmaceutical industry CEO's, sometimes in the WH basement and sometimes at offices down the street fromt he WH.
In return for their hard work, Emanuel will never have to worry about campaign contributions to run for any office he wants, and currently he is the mayor of Chicago.
And Fowler was awarded a plum and cushy spot inside WellPoint Insurance as soon as Congress and the President got the 2,000 page travesty passed and signed.
I wish I could be optimistic that some day soon, we will have ourselves some real health care reform, but with the insurance industry now having even more money than before, so it can buy even more Congressional puppets,. I am not holding my breath.
RobinA
(10,291 posts)A long time poster writes that his wife is having a hard time getting a drug she needs for her serious, chronic disease and a significant percentage of the responses take him to task for calling the President a bad word. Yikes. This has become a truly nasty place.
pnwmom
(109,801 posts)That insurance agent-friend fed him a pile of crap and he swallowed it.
No wonder there are so many people who don't understand the law, if even Will could be misled.
The lies Will swallowed:
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686037
There are ten different health insurance companies in NH. According to the independent (family friend, ally) insurance adjuster I spoke to at length this afternoon, pursuing coverage with any of them would be a waste of time. Why? Because - according to dude - the whole "You cannot deny coverage to people with pre-existing conditions" thing only applies to insurance companies within the ACA network. You heard all that shit about "Grandfathering." Well, this is that, and all of them will turn us down because they still can.
I am in the process of running down the facts of the matter, but family friend and ally was confident enough to basically tell us not to bother.
So yeah, that, too.
___________________
The facts:
http://www.nytimes.com/2013/10/26/your-money/health-insurance-options-arent-limited-to-obamacare-exchanges.html?_r=0
In general, health policies effective Jan. 1, whether sold on the exchanges or off, must comply with the Affordable Care Act. That means they have to offer the same menu of essential benefits, like drug coverage and maternity care, and can’t deny you coverage if you’re already sick. And, insurers who sell policies both on and off the exchanges must sell the same plan for the same price.
http://www.insure.com/articles/healthinsurance/buying-health-insurance-outside-exchange.html?WT.qs_osrc=fxb-182807210
Drug coverage
Drug coverage is yet another variable. You may find you have more options when it comes to drug coverage if you shop off-exchange. Like provider networks, health plans can limit the drugs that are covered, or reimburse more for generics than brand-names, or reimburse more for drugs you buy mail-order than from your local pharmacy.
If you have a health condition and use a particular drug, you should check that it's covered under the plan in which you want to enroll, whether that plan is on the exchange or off-exchange, Coleman advises.
Remember, too, he says, the cap on out-of-pocket expenses doesn't apply to drugs not on a health plan's list of covered medications.
brush
(59,431 posts)on this allegedly progressive site.
It's really now more like 50% progressive. I won't say what the rest are but this place has certainly changed over the years — especially the last 5 years 2 months.
laundry_queen
(8,646 posts)but I'm in Canada, with single payer and we still have to deal with the assholes at the insurance company for meds. Most meds aren't covered unless you are very poor, or a senior, or a kid in poverty. However, at least we have some cost control so that when we do have to pay out of pocket for a med, it's normally somewhat affordable. Still, there was a bit on the news not too long ago that showed how having cancer could basically ruin someone financially in Canada due to oral chemo not being covered 100% like IV chemo in the hospital is. Single payer should include drug and dental coverage too, IMO. Insurance companies are a pox on society. Hope you find a solution soon.
Lex
(34,108 posts)Even before Obamacare certainly. It sucks.
TrollBuster9090
(6,053 posts)As I understand it, there is no cure or treatment for Multiple Sclerosis, and its etiology is not fully understood. There are only treatments for the symptoms, and they are usually pretty standard and cheap (ie-corticosteroids during episodes etc.). If you asked for an experimental drug that hasn't yet been conclusively proven to be effective, of course they wouldn't pay for it. They wouldn't pay for it even in a country that had a single payer healthcare system.
Just curious. So, what specifically did you ask for that was denied?
Lex
(34,108 posts)Copaxone, Avonex and Betaseron are all standard meds for MS and run about 16K or so per year, if not more.
TrollBuster9090
(6,053 posts)possible that insurance companies will pay for generic versions, but not brand name formulations?
Lex
(34,108 posts)Insurance pays for my partner's Rebif, and before that, paid for her Avonex.
There could be generics now, but not sure.
TrollBuster9090
(6,053 posts)I don't know either. But this sort of thing happens a lot when someone switches from one plan to another, and the new provider won't pay for the drug they're used to; but will pay for either a cheaper formulation, or an alternative (cheaper) treatment that's been proven to be roughly as effective. People automatically think they're being 'denied treatment' because they're being denied the specific thing they're used to, as opposed to something that is considered 'equivalent' but cheaper. And that happened long before Obamacare. *Shrug*
Lex
(34,108 posts)that particular drug, and that the patient tried the other medicine on the patient and it didn't work as well. Appeals can work.
blindersoff
(258 posts)there are no generics for any of the disease modifying drugs as far as I know. The cost of producing them is far less than they charge the patient (Avonex cost to the patient without insurance would be about $4000/mo). But I think that most of the companies who produce these drugs want patients to stay on them and so are willing to assist with copays. My copay for Avonex is $10/mo after being $175/mo. All I had to do was request it, they reviewed it and I got it!
TrollBuster9090
(6,053 posts)Glad that worked out for you. I'm just wondering if their 'review' of your copay was related to the copay limit that was imposed on them by the ACA. I suspect it was.
Response to WilliamPitt (Original post)
Post removed
Oilwellian
(12,647 posts)Using this thread to take pot shots at Will is BEYOND disgusting.
![]()
Whisp
(24,096 posts)as if Obama personally intruded to make life harder for the OP.
jesus.
![]()
panader0
(25,816 posts)You can call Obama a piece of shit and not get hidden. But offend Will and......
1000words
(7,051 posts)Taking the opportunity to tell Will to "grow up" and lecturing him on how to properly express his anger.
brush
(59,431 posts)This is not freeperville.
the_sly_pig
(751 posts)One's health is important. We have bought into this falsehood of 'choice'. Choice regarding healthcare is a myth. I choose to go to a doctor to improve my health, end of story.
It doesn't matter what doctor, it doesn't matter the prescription. Go to a doctor, get a prescription, get healthy or at least maintain your health.
Any plan that doesn't cover this or doesn't cover that is trickery as is 'choice'.
We're missing the big picture here. Health care is not a choice, it's a right. The sick are profitable, and those making money from the sick are scum.
Oilwellian
(12,647 posts)I could just cry. ![]()
djean111
(14,255 posts)Having insurance does not mean you will get affordable health care.
You will just have insurance.
steve2470
(37,468 posts)obliviously
(1,635 posts)MineralMan
(148,792 posts)I recommend a self deletion.
greytdemocrat
(3,300 posts)Asked for your head yet??? ![]()
I hope it works out for your wife.
Glimmer of Hope
(5,823 posts)They do this intentionally because they know some will give up out of frustration or not follow-up. You have to push them until they give what you need.
It is the insurance industry that is a POS.
rudolph the red
(666 posts)It's almost like you are magic, man.
Whisp
(24,096 posts)I wish we were all that special.
panader0
(25,816 posts)I carefully informed the buyer of it's pre-existing conditions. Am I a POS now too?
lostincalifornia
(3,639 posts)Suggestion would be is if appeals do not work he should try a Canadian pharmacy
Hissyspit
(45,790 posts)1.) Your analogy makes no sense at all. The pre-existing condition relates to the buyer.
2.) OP is clearly referring to dishonest car sales tactics.
panader0
(25,816 posts)I'm blown away that apparently now, anyone can say anything on DU. Or at least, some people. I notice that Pirate Smile's post was hidden--was it more offensive than the OP?
PS, not all used car salesmen are POS.
KoKo
(84,711 posts)Last edited Tue Mar 18, 2014, 09:17 PM - Edit history (1)
thought your wife could have gotten her meds by now and to see this from you...
What can one say?
THIS SHOULD NOT BE!
Holly_Hobby
(3,033 posts)My husband gets his gout med here and it saves us $529/month! Very nice people, easy to work with.
http://www.northwestpharmacy.com/
Indykatie
(3,853 posts)Was it covered by insurance or deemed investigational or not covered for some other reason?
magical thyme
(14,881 posts)but they lived in Massachusetts at the time.
MADem
(135,425 posts)MA has state income taxes, though--NH does not.
Texasgal
(17,211 posts)In fact it has many flaws. I am so sorry for your wife. I hope you can find the help she needs.
I never thought ACA was the end all to all of our healthcare issues. It's an okay program not perfect by any stretch.
bvar22
(39,909 posts)but WE had to have a "Uniquely American Solution"
where access to Health Care is a COMMODITY to be SOLD to Americans by For Profit Corporations.
These opportunities like we had in 2008 come along only once in a generation.
WE are going to be stuck with this Uniquely American Solution for a LONG time.
FDR and LBJ are crying in their graves.
[font color=white]......[/font][font size=4]Obama's Army for “CHANGE”, Jan. 21, 2009[/font]

[font color=white].....................[/font][font size=4]"Oh, What could have been."[/font]
woo me with science
(32,139 posts)jsr
(7,712 posts)etc. etc. ![]()
marble falls
(64,371 posts)Cofitachequi
(112 posts)Their Freepathon is over, but you will have an opportunity to contribute in the next few weeks.
Hissyspit
(45,790 posts)lostincalifornia
(3,639 posts)Whisp
(24,096 posts)all kinds of shit with blessing.
bobduca
(1,763 posts)tell everyone why Will is wrong to feel the way he does about his experience.
lostincalifornia
(3,639 posts)OP
LiberalAndProud
(12,799 posts)Post hidden and OP locked out. There won't be any more responses on this thread from him.
brush
(59,431 posts)getting her medication.
On DU he SHOULD NOT have the right to call the President "a piece of shit."
That's not that hard to understand. He's also went off mistakenly before on the President. See post 476.
AnalystInParadise
(1,832 posts)saying F.U. is the least I would do. Cut the guy some fucking slack, I swear it is like people have their god damn humanity removed when someone attacks a sacred totem of any stripe.
I don't even like Will Pitt, we do not get along, but this is his wife suffering because of the ACA, I can't fault his anger and fear.
ProSense
(116,464 posts)"I don't even like Will Pitt, we do not get along, but this is his wife suffering because of the ACA, I can't fault his anger and fear."
...absolutely nothing to do with "his wife suffering." It's a horrible situation, but this OP is simply an attack on the President from an uninformed perspective.
Formularies are not determined by the President, and existed before ACA. They exist in Medicare Part D.
The bizarre thing about attacking the President and Obamacare is that the law did improve the situation.
The Affordable Care Act ensures your right to appeal health insurance plan decisions--to ask that your plan reconsider its decision to deny payment for a service or treatment. New rules that apply to health plans created after March 23, 2010 spell out how your plan must handle your appeal (usually called an “internal appeal”). If your plan still denies payment after considering your appeal, the law permits you to have an independent review organization decide whether to uphold or overturn the plan’s decision. This final check is often referred to as an “external review.”
http://www.hhs.gov/healthcare/rights/appeal/appealing-health-plan-decisions.html
AnalystInParadise
(1,832 posts)if you didn't act like a know it all jackhole, I would take you more seriously, but you literally can never be wrong, even when people beat you in the head with the truth and facts.
Good day sir.
ProSense
(116,464 posts)AnalystInParadise
(1,832 posts)n/t
ProSense
(116,464 posts)AnalystInParadise
(1,832 posts)and don't seem to have a fetish to defend the indefensible. But I await your next piece of performance art comedy gold where you lie, spin and do anything you can to deny admitting you are ever wrong. ![]() Cheers.
Cheers.
sheshe2
(91,012 posts)and damn close to an alert if it has not already been done.
Good day sir.
jackhole
Portmanteau of "Jackass" and "Asshole".
Originated as a name by radio personalities Kevin and Bean (from KROQ-FM in Los Angeles) as a way of calling somebody a nasty name without actually breaking FCC edicts against foul language.
http://www.urbandictionary.com/define.php?term=jackhole
and don't seem to have a fetish to defend the indefensible. But I await your next piece of performance art comedy gold where you lie, spin and do anything you can to deny admitting you are ever wrong. Cheers.
Re read your posts and consider deleting them. You just called ProSense a Jackhole that lies and spins a story. You just called out a DUer. Do you care to reconsider your statements?
I await your response.
AnalystInParadise
(1,832 posts)You doing what you THREATEN proves my point, so please take your threats elsewhere.
sheshe2
(91,012 posts)That is a fact. And it is against DU rules.
I did not threaten you, I tried to explain some facts. You are over the line here. How putting threaten in caps proves your point, I have no clue.
AnalystInParadise
(1,832 posts)Point proven, and thanks for playing.
sheshe2
(91,012 posts)You answered it all.
It is all a game to you. Got it.
ProSense
(116,464 posts)"But I await your next piece of performance art comedy gold where you lie, spin and do anything you can to deny admitting you are ever wrong. "
...you think the drivel you post are gems of wisdom. I'll admit I'm "wrong" when I'm wrong. As of this post, the OP is still fly paper for those who want to attack the President based on inaccurate information.
I'm sure that's why you're making it known that...
"I don't even like Will Pitt, we do not get along..."
http://www.democraticunderground.com/10024685964#post314
"I don't like Will"
http://www.democraticunderground.com/10024685964#post372
![]()
AnalystInParadise
(1,832 posts)links to the original post are a rebuttal to a complex discussion? I am not even upset with you, now I just feel sorry for you and your can't color inside the lines third grade logic. It's all good Prosense, I understand now.
ProSense
(116,464 posts)"I am not even upset with you"
![]()
JEB
(4,748 posts)are capable of.
bvar22
(39,909 posts)I would rather shoot myself in the head than to start running MY life based on what FreeRepublic, or Rush,
or what The Republicans think.
Nice to know you are spending your time there.
Whisp
(24,096 posts)but it bothers you for the Name to be even spoken here?
meh, Freeper links are a staple here for a long time. Funny how it's suddenly a verboten site to link to.
AnalystInParadise
(1,832 posts)Does that site have a trademark on certain words, or is this some bullshit character assassination thing you are peddling....
Whisp
(24,096 posts)but maybe you are right, Freepers probably don't call the President a piece of shit used car salesman. I'm just guessing, I sure could be wrong but I see what the OP said.
truedelphi
(32,324 posts)Real true health care reform
Punishing the war criminals of the Bus/Cheney regime
Punishing the Big Bankers and Big Financial People, instead of handing Main Street's wealth over to them
Etcetera
Then it would not be happening that people would be using "anger words" in reference to him.
Some of us lived during the FDR era. Others here remember our parents and grandparents talking about FDR. He actually went into the halls of Congress and called for a 100 day Congressional session to address what was happening in terms of the Depression-era economy. This President pretends there is no Depression.
bvar22
(39,909 posts)....without having to rely on FreeRepublic.
But if YOU need to use FR as a vocabulary and idea resource, I won't stop you.
Go get you some!!!
Don't be surprised if I or other Liberals at DU don't care what you find on your expeditions.
Maybe you can confine FR reposts to The BOG where we won't have to see it.
I really, REALLY don't care what FR or other Conservatives have to say,
and MY life won't change one whit based on what is written there.
I can't speak for Will,
but I will bet that he doesn't care either.
Whisp
(24,096 posts)yah, right.
only the chosen can do that.
1000words
(7,051 posts)I know I just happened to come upon FR threads all the time.
![]()
lostincalifornia
(3,639 posts)Discussing the problems of the ACA that one has to call the President names and say some of the most disgusting expletives about the President, instead of criticizing it in a normal way
This isn't the first time I have seen it, and it does a disservice to DU
Whisp
(24,096 posts)whether others have gone through the same thing. It could have been a very valuable learning process (lots and lots of good advice here in this thread) but what it is is a big pile of stinkin' shit.
AnalystInParadise
(1,832 posts)Who gives two flying fucks what the "kids" in the other clique think? The man's wife is suffering and the ACA is at least part to blame. Since this is PBO's signature achievement, I don't consider it flawed for the man to vent a primal scream at the law and the President because his wife is suffering. People alerting on him and calling him out because his wife is suffering and he is upset, fearful and stressed make me want to fucking vomit. Yeah some of you are real fucking progressives.......I would not have said what he said, but I understand the pain and fear he is displaying and will cut the guy some slack.
jeff47
(26,549 posts)1) Post an angry rant screaming at everyone.
2) Talk about his problem and ask for advice.
He did 1, got locked out of his own thread, and ended up with a thread full of shit.
If he did 2, he would have had the posts showing him where to go to appeal the decision and get the drug. There's a few of them sprinkled in this thread, but they're hard to find among the shit.
#2 would have solved his problem. He did #1.
bobduca
(1,763 posts)also why the fuck are you over there?
lostincalifornia
(3,639 posts)Over the top
That is not the way to criticize a program or the President
bobduca
(1,763 posts)but then many Du'ers also know the score and ignore fox.
hint: the enemy of the 99%, its not just Brit Hume.
lostincalifornia
(3,639 posts)Whatever the reason it isn't because they subscribe to those views. Perhaps to convey to those who don't watch that crap just how over the top they are
As for your question, you will find various posts from DUers linking those sites. It does not appear rampant but it does happen, and it is even more frequent on faux links
Whisp
(24,096 posts)Hissyspit
(45,790 posts)On edit:
If I'm recalling correctly, at one time you were not allowed to link there, but it may have been a ban on mentioning the name. I just don't quite remember, but others probably will.
LiberalAndProud
(12,799 posts)There is a cave that was not allowed to be mentioned or linked.
I guess I have just missed those threads... and now i need a shower and an anti-virus scan for clicking on that.
Whisp
(24,096 posts)is what I understand.
kind of a Hatfield and McCoy rivalry thing.
DebJ
(7,699 posts)i joined DU in October, 2003, after many months of 'lurking'. FR posts used to be linked to quite regularly here.
They were a source of some amusement combined with disgust and ultimately sometimes fear that such people actually
exist in this country. I clicked on the link because I haven't seen their site for many years now, and I wanted to see
if it was still in that hideously primitive condition.........it is. At one point I think they were about to shut down from lack
of funding.
Anyway, it was no big deal then. I don't understand why it is a big deal now............. who cares?
hrmjustin
(71,265 posts)passiveporcupine
(8,175 posts)For more information, please contact MSAA's Client Services Helpline at (800) 532-7667, extension 154, or email MSquestions@mymsaa.org.
http://mymsaa.org/about-ms/aca/non-medicare/
Whisp
(24,096 posts)he/she sounds like a ron paul fucker or a repug to mislead and misinform.
pnwmom
(109,801 posts)pnwmom
(109,801 posts)And are you going to appeal? There is an appeals process.
I'm so sorry to hear about this happening to you. This is terrible.
Response to pnwmom (Reply #293)
DebJ This message was self-deleted by its author.
pnwmom
(109,801 posts)of the other insurers, both on and off the exchange.
DebJ
(7,699 posts)plan you signed up for has not yet begun, only if the effective date is still pending.
I'm going to delete my original post so no one picks up my bad info, thanks!
phleshdef
(11,936 posts)I feel bad for your wife. But your uncalled for attitude and lack of critical thinking when writing your OP can eat a bag of dicks.
lostincalifornia
(3,639 posts)Thread from the OP, and more of flame bait then useful criticism, and then figuring out what options exist
phleshdef
(11,936 posts)But its worth it. The OP crossed the line for me because I know that he knows better. And I believe there are probably options that would allow his wife to get what she needs, but he doesn't wanna talk about that. He wants to use it as an opportunity to talk down to Barack Obama using subhuman terminology.
lostincalifornia
(3,639 posts)phleshdef
(11,936 posts)Fuck Obama for helping millions of people get access to imperfect insurance that still saves a lot of lives when it matters.
Fuck that piece of shit car salesman for funding thousands of free clinics, for establishing the best access to birth control women have ever had, fuck that dirty DINO trash for the ACA... obviously because it didn't solve all of Will Pitt's problems, it means Obama is nothing but a corporate whore that didn't do anything for anyone.
Hoyt
(54,770 posts)However, I do understand anger over what a family member is going through and hope the drug situation gets worked out.
Obama has helped a lot of folks, and it took guts to even tackle health care after what happened to Hillarycare. The people that deserve ridicule are the ignorant voters who didn't call their conservative representatives supporting better legislation.
Raven
(14,225 posts)pnwmom
(109,801 posts)and now he's repeating it here. The fact is that all insurers, both on and off the exchange, must take all comers. They can no longer deny people due to preexisting conditions. But the only place you can get a subsidy is on the state or Federal exchange.
I completely understand how stressed out by this situation with his wife, but he needs to take some positive steps now.
Investigate the drug formularies of all the plans that are available to him, both on and off the exchange. If he finds one that works better, than cancel this policy and buy a new one. He still has some time but he has to act fast.
Immediately appeal this insurer's decision, if he hasn't already done so.
With so little time, I'd work on both fronts.
http://www.nytimes.com/2013/10/26/your-money/health-insurance-options-arent-limited-to-obamacare-exchanges.html?_r=0
In general, health policies effective Jan. 1, whether sold on the exchanges or off, must comply with the Affordable Care Act. That means they have to offer the same menu of essential benefits, like drug coverage and maternity care, and can’t deny you coverage if you’re already sick. And, insurers who sell policies both on and off the exchanges must sell the same plan for the same price.
http://www.insure.com/articles/healthinsurance/buying-health-insurance-outside-exchange.html?WT.qs_osrc=fxb-182807210
Drug coverage
Drug coverage is yet another variable. You may find you have more options when it comes to drug coverage if you shop off-exchange. Like provider networks, health plans can limit the drugs that are covered, or reimburse more for generics than brand-names, or reimburse more for drugs you buy mail-order than from your local pharmacy.
If you have a health condition and use a particular drug, you should check that it's covered under the plan in which you want to enroll, whether that plan is on the exchange or off-exchange, Coleman advises.
Remember, too, he says, the cap on out-of-pocket expenses doesn't apply to drugs not on a health plan's list of covered medications.
JEB
(4,748 posts)DebJ
(7,699 posts)for his wife, but coverage for the life-saving medicine she requires is denied, so he ends up in almost the same situation
as if he didn't have the coverage.
I might be having a senior moment here, but didn't Will post at one point that his wife had to use this specific medicine and that it wasn't a common one, that other meds didn't work for her? Lots of people are posting about a wider array of meds available for MS, but I think he already said those didn't work for her.
Not that I defend his attack on the President.
I do, however, have great empathy for the absolute terror of not having the medicines or medical care that is desperately needed, particularly when the difference is life-and-death. Been there, done that, and may soon face it again.
pnwmom
(109,801 posts)"There are ten different health insurance companies in NH. According to the independent (family friend, ally) insurance adjuster I spoke to at length this afternoon, pursuing coverage with any of them would be a waste of time. Why? Because - according to dude - the whole "You cannot deny coverage to people with pre-existing conditions" thing only applies to insurance companies within the ACA network. You heard all that shit about "Grandfathering." Well, this is that, and all of them will turn us down because they still can.
"I am in the process of running down the facts of the matter, but family friend and ally was confident enough to basically tell us not to bother.
"So yeah, that, too."
JVS
(61,935 posts)phleshdef
(11,936 posts)What is different about this situation and how is it that Obama is to blame?
Logical
(22,457 posts)pnwmom
(109,801 posts)and Will was understandably disturbed.
He needs a new agent.
What the agent said:
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686037
What the facts are:
http://www.democraticunderground.com/10024687956
phleshdef
(11,936 posts)pnwmom
(109,801 posts)pnwmom
(109,801 posts)agent.
They need to fire that broker and find another one, quickly. He lied to them about insurers outside of the exchange being able to bar people with preexisting conditions.
http://www.democraticunderground.com/10024687956
SidDithers
(44,331 posts)Sid
msanthrope
(37,549 posts)advice by this 'agent' and he should thank her for it.
Logical
(22,457 posts)alarimer
(17,071 posts)I'm afraid we were sold a bill of goods. And people will suffer as a result.
My sister has MS as well. He company dropped drug coverage a while back, to avoid the high costs of covering people like her. She must have found a way because she seems to be doing all right.
JEB
(4,748 posts)when you or your family is the disaster. The array of complex and deceiving policies are all designed to maximize profit when disaster hits.
Response to WilliamPitt (Original post)
krawhitham This message was self-deleted by its author.
killbotfactory
(13,566 posts)JEB
(4,748 posts)about a offensive remark toward the President than they do about the life and well being of a living breathing person. Shameful.
pa28
(6,145 posts)I'm glad you called it shameful because surprising would be the wrong word.
Bobbie Jo
(14,344 posts)"concern" and "disgust" from the usual people. Equality unsurprising and hollow.
pa28
(6,145 posts)Last edited Wed Mar 19, 2014, 01:37 AM - Edit history (1)
The ACA is a Republican concept. It's not going to be fixed or repaired.
"Nixoncare" aka "Heritagecare" was conceived to head off a government run, single player healthcare system by institutionalizing private insurers.
The part that needs fixing is the actual foundation of the plan. Private, for profit insurance companies exist to deny care. That's the point and it's going to stay that way.
Healthcare should be a basic right in any advanced economy. We had our chance to clean out the scum and we blew it.
minivan2
(214 posts)I understand why you're upset, I would be too. But calling the president a "piece of shit used-car salesman." Is way too much. I think that you should delete your post, take a breather and apologize for the rant.
woo me with science
(32,139 posts)especially when it involves so much personal pain.
Nothing changes until we are collectively honest about the level of corruption we *really* face, and the pain it *really* causes...all the propaganda be damned.
I can't express enough how sorry, and angry, I am that this is happening to your wife and your family.
Cali_Democrat
(30,439 posts)This pathetic OP or the fact that you're running around with a Bernie Sanders sig even though he voted for the bill.
![]()
woo me with science
(32,139 posts)Cha
(309,260 posts)this misplaced anger on the President to get their raging "fuck you" hate on..



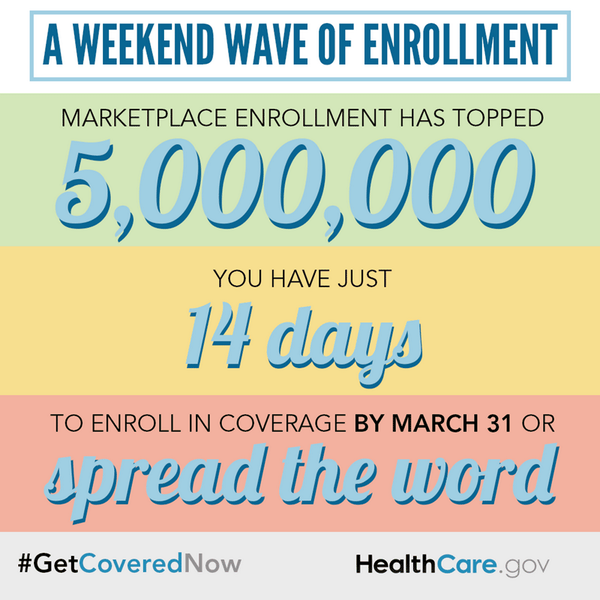
Lars39
(26,351 posts)Hope to goddess you're never faced with their rock or hard place situation.
Cha
(309,260 posts)is fair game.
Lars39
(26,351 posts)You have groused more about a man venting at his wife's reality than you have shown compassion for their predicament.
Cha
(309,260 posts)Yeah, really something to be REC.. Ignorance is not bliss.
Lars39
(26,351 posts)I don't believe you comprehend that this isn't a game.
Cha
(309,260 posts)"Or... you can carry on without insurance, never getting to see a doctor, and die from the high blood pressure you didn't know you had.
I have been denied insurance for over 12 years. Scratch that...I was offered a 'plan' for $1200/mo that included a rider that excluded coverage for pretty much everything except falling out of my car. I now have a plan for $75/mo that doesn't exclude a damned thing and also covers meds for 50% of cost. Granted, it's been so long since I've been able to see a doctor that I'm absolutely terrified to go, now. But, I will...eventually. And, I will be grateful that I have insurance that will cover any catastrophic issues that may come up.
What Will is going through is tough, but he's received some helpful advice that he doesn't seem to want. I guess it's easier to be angry than actually fight. A lot of people are seeing real benefits from the ACA. Like everything else, this will be improved over time.
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686725
Bolding is mine.
Lars39
(26,351 posts)"Tough" ? Devastating, when the cost of a family's insurance and medicine will keep them poor or near enough.
Cha
(309,260 posts)Aerows
(39,961 posts)Because you are probably in for an unpleasant surprise.
rudolph the red
(666 posts)He gets a pass.
Cha
(309,260 posts)His Magic Man Fans weren't on that jury.
JI7
(91,658 posts)considering his recent threads i think he is just looking for attention and hoping for support from a certain crowd.
as others have pointed out this case with the meds has always happened, even before Obama. and he is living in a state without state income taxes. maybe he should consider getting some change in that area so they can support more govt programs to help with these type of things.
Cha
(309,260 posts)misplaced ugly, bitter, insulting temper tantrum on Pres Obama.
Sounds like New Hampshire does need some changes to help those who can't afford expensive meds. No income tax?! how do they fix roads, have libraries, pay teachers..?
Whisp
(24,096 posts)but it's been fucking consistent against the President for a long time now. Dripping with rage and hate and misinformation. Grabbing at any chance to shit on him.
so no, no pass.
there is something going on here with this one.
Cha
(309,260 posts)I wouldn't give him a pass if it were his very first raging "Fuck You, Obama" screed. And, they're always from his "heart and soul", right. fooking drama monger.
giftedgirl77
(4,713 posts)the POTUS, yet conveniently forgets to lay any of the blame with the damn pharmaceutical companies that not only monopolize these specialty medications but fix the prices as well.
P.S. love teh kitteh ![]()
Vashta Nerada
(3,922 posts)Shame.
AnalystInParadise
(1,832 posts)And I mean that sincerely.
ucrdem
(15,720 posts)Now I'm told you're locked out of this thread so I'll say no more.
JI7
(91,658 posts)MisterP
(23,730 posts)it needs fixing at all
it's like sitting on a cactus
ohheckyeah
(9,314 posts)seems to think I can afford. And of course, since I'm a smoker I don't in their eyes deserve to have health insurance. They don't ask if you drink or how much you weigh, just if you smoke. The ACA doesn't do me a damn bit of good.
And save the sermons about cigarettes...you don't know my situation.
VanillaRhapsody
(21,115 posts)ohheckyeah
(9,314 posts)Virginia isn't as red as it used to be.
Drunken Irishman
(34,857 posts)It sounds like you didn't do your due diligence. It sucks, but you're a smart guy, I would expect that you would have looked up what the plan covered before plopping down $700 a month on it. If you had any questions, you could have gone to a broker would would've been able to guide you through the process so you didn't enroll in a plan that doesn't work for you.
Moreover, what did you do between the time you enrolled in the plan and the plan started? Because there is a wide window for you to research the plan to make sure it's the right one and then make the needed changes so that you can get a plan that covers your wife's medication.
I know this because plans do not start the second you enroll. If you enrolled between Oct. 1st and Dec. 24th, your plan started on the 1st of the year - that gave you a pretty significant window to shop for the right plan. If you enrolled after Dec. 24th and through to Jan. 15th, your coverage wouldn't have begun until February 1st. That gave you two and a half weeks to make sure everything was covered in your plan before its plan start date. If you enrolled any time between January 16th and February 15th, your coverage began on March 1st - which, again, gives you roughly two weeks at the latest to change your plan. The same goes for February 16th to March 15th (for your plan to start on April 1st).
You should have checked the plan and spoke with your doctor, and your pharmacist, everything was covered. It's not that hard.
JEB
(4,748 posts)is very hard. Insurance agents are only interested in selling, selling, selling their favored products. A shifting sea of variables and deceitful language. $700 hundred fucking dollars should provide for any coverage needed. Fucking criminal.
Drunken Irishman
(34,857 posts)It's not that hard. You can even look up the information on your own through healthcare.gov. It looks like the OP pretty much just enrolled without even checking to see what the plan covered. It sucks, but he had plenty of time to make sure it was the right plan.
JEB
(4,748 posts)Tried numerous times via the computer. Hours wasted. Drove an hour and a half each way to an event to try and enroll. Called various State officials, called various insurance agents. Called various insurance companies. Received someone elses application from Cover Oregon. Called Cover Oregon, waited for over an hour on hold. Was told everything would be fixed and to expect the correct papers in the mail. Waited two weeks called again waited over an hour again. Finally got someone who seemed to know what to do. I signed up for the cheapest thing they offered (very high deductible). Never received anything from the insurance company. Called them, waiting over 45 minutes to be reassured everything was on track. Still haven't received a bill. Was shooting for January first coverage.
Drunken Irishman
(34,857 posts)It's unfortunate, but it's the nature of the beast. I guess he'd rather we just go back to the old system where EVERYONE was fucked.
Basically, it's all or nothing with some people.
JEB
(4,748 posts)to get the medicine she needs.
pnwmom
(109,801 posts)This is a cost that must be reined in, but it's one more thing that the Rethugs are resisting. We tried to pass a bill allowing Medicare/Medicaid to negotiate with drug companies for better prices (as Canada does) and the Rethugs opposed it.
Puzzledtraveller
(5,937 posts)to real consumers and clients, I give a hearty K&R.
pnwmom
(109,801 posts)when he claimed that insurers outside the exchange can reject people for preexisting conditions? If you are really marketing these plans you must know that isn't true, right?
And you are aware that both private insurance plans and single payer plans (such as Medicare, Canadian Single payer, and UK single payer) use formularies? That, under the ACA, there is now an internal appeals process, and external appeals process, and a process for requesting exceptions? I hope so, if you really do sell these plans all day.
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4686037
There are ten different health insurance companies in NH. According to the independent (family friend, ally) insurance adjuster I spoke to at length this afternoon, pursuing coverage with any of them would be a waste of time. Why? Because - according to dude - the whole "You cannot deny coverage to people with pre-existing conditions" thing only applies to insurance companies within the ACA network. You heard all that shit about "Grandfathering." Well, this is that, and all of them will turn us down because they still can.
I am in the process of running down the facts of the matter, but family friend and ally was confident enough to basically tell us not to bother.
So yeah, that, too.
http://thinkprogress.org/health/2013/12/10/3042741/drugs-obamacare-coverage/
But yes, there are certain limits: a formulary, for instance, may cover three drugs for treating a certain condition but not two others. Obamacare — like all insurers currently operating in the market — has a fix for that. ACA regulations demand that a health plan must have an “exceptions process” in place that allows patients to request and gain access to clinically appropriate drugs that aren’t covered by the health plan (in addition to internal and external appeal processes). So, if a health plan does not cover a particular drug that a patient absolutely needs, their doctor can certify medical necessity to extend coverage. Insurers have relied on drug formularies before the law went into effect and already have exceptions processes in place, meaning that most “will not have to implement significant changes.”
In his piece, Gottlieb illustrates the narrowness of some formularies this way: “I found one plan in North Carolina that doesn’t cover Actonel for osteoporosis, Aubagio for multiple sclerosis, or Xeljanz for severe rheumatoid arthritis, among other ‘non formulary’ drugs.” But as Washington & Lee law professor Tim Jost points out, “This is the way formularies work, we’ve decided we’re going to cover these drugs, but not those drugs… I don’t think you can know anything from seeing what they list as the non formulary drugs without knowing what the formulary is and how fungible those drugs are with the formulary drugs.” Jost notes that drugs within the same category and class are more or less fungible, and so for most people, the drug that’s offered will work as well as the one that isn’t — and is often far cheaper than the name brand option.
Cha
(309,260 posts)like you really hate your job. That's too bad.. maybe you could find something more suited to you so you wouldn't have to "peddle" something you didn't like. You wouldn't have to be so fake.
Glitterati
(3,182 posts)Fight! Don't stand down. The harder you fight, the more determined you are, the louder you complain the faster this is going to be resolved.
And, it WILL be resolved.
Your wife's doctor should be your strongest ally in this. S/HE should be the soldier standing at the front lines fighting for your wife's patient care beside you.
I have the same thing (not as expensive) with one of my meds - the insurance company wants me on a cheap, generic drug. But, my doctor led the fight as far as the drug companies and the cheap, generic drug was just pulled off the market, so the only drug available now is the one I am on. But, it was the medical community that went to the authorities and explained that the cheap, generic drug didn't WORK.
SomethingFishy
(4,876 posts)I don't understand why you don't just quit your job, and spend all your time trying to get useful insurance. From reading through your thread that seems to be the answer to your problem. You just aren't spending enough time "shopping".
If you quit your job you should have plenty of time to wade through a system specifically designed to give you as little care as possible for the most amount of money so we can maintain our "capitalist integrity" and continue to use the health of our citizens as profit making enterprise.
Commie. ![]()
Le Taz Hot
(22,271 posts)telling me "you don't understand" or "you're misinterpreting it" that I could spit. I went over every inch of this program before I signed up and it's the apologists that don't or refuse to understand the "exceptions." There are so many holes in the ACA, a COMPLETE capitulation to the insurance companies, it's pathetic. I'm shelling out $300.00 a month for insurance I'll never be able to use. I know $300.00 a month doesn't sound like a lot to most people but it's an incredible sacrifice to us. The apologists like to come back with the "well, it's better than nothing!" No, not it's not. Because between having no insurance and being low income I could get FREE meds through the manufacturer and a HUGE discount on the ones that weren't free through Walgreens pharmacy. Now I have "insurance" and, because of a $6,000 a year deductible, per person, I'll have to pay full price which isn't going to happen because ONE medication is $300.00 a month. ONE. My husband takes 3 and I take 2. Full price we're looking easily at $600.00 a month or more and that's on top of the $300.00 a month give away to the insurance companies.
ProSense
(116,464 posts)"I'm shelling out $300.00 a month for insurance I'll never be able to use."
If you're not going to use it, why pay for it? Save the money and pay the penalty.
"I am SO sick and tired of the apologists"
Informing people about the facts is not being an "apologist"
Don't be deceived. Contrary to popular opinion, ALL insurers, whether on or off the exchanges
http://www.democraticunderground.com/10024687956
Le Taz Hot
(22,271 posts)That seems to explain it all for you people. I'm done here.
ProSense
(116,464 posts)truebrit71
(20,805 posts)...
NCTraveler
(30,481 posts)and the manner in which this bill was sold to the people. Lie after lie was foisted on to the American people. That being said, many people will be helped by it. Many. I have been pretty critical of the ACA. I think the whole concept goes against what Democrats should stand for. I felt the same way about HillaryCare. The political clout needed to push something so weak and against Democratic principals was simply too much. What came out in the end is too weak for what transpired. I still keep trying to go back to the fact that it will help many people. It has actually hurt someone I know yet they are willing to accept it without a fight. My heart goes out to you and your situation.
Response to WilliamPitt (Original post)
Post removed
Response to Post removed (Reply #528)
Hissyspit This message was self-deleted by its author.
Hissyspit
(45,790 posts)Ugly. Says way more about you then Will Pitt.
Even if one doesn't agree with what the OP says.
joshcryer
(62,515 posts)He actually responded to a post I wrote today. I respect his opinion.
But he got banned from DU for threatening the life of another poster. It was one of the very rare (handful of?) instances where a ban was overturned.
I sincerely mean it. Emotions expressed on a forum are nothing. If there is even a 10% amplification in real life, some people here need to control it. ![]()
ScreamingMeemie
(68,918 posts)fleabiscuit
(4,542 posts)We have had the experience where our insurance covered a med for wife with $50 co-pays, then with a stroke of a pen it went to $1000. Back to alternative that didn't work as good. I don't think there is a county in the world that will cover all medication, especially new or experimental ones. Sigh.
wordpix
(18,652 posts)This is about cancer but check it out for MS.
Autumn
(47,627 posts)It's really quite hilarious to see the contortions to prove you are wrong and just BAD. BAD
rtracey
(2,062 posts)Man...this joint is becoming too radical for me...I'm heading out the door on Democratic Underground. When I joined, this place was always respectable to our leaders... but not now....screaming F.U. to our president, really....hey you can have it. The administration on this site has taken a back set to a lot of stuff....too bad......seeya
LexVegas
(6,679 posts)However, I don't see how the President is in any way responsible for the denial of coverage on the meds.
AngryAmish
(25,704 posts)ramapo
(4,760 posts)The answer is easy, no ACA.
There are many deficiencies in the ACA, chief of which is it goes nowhere near far enough to reign in the insurance companies.
There are no requirements that they offer individual policies in a state where they write group insurance. So here in NJ we have a distinct lack of choice. There is little to require broad networks and nothing to require PPOs which provide out-of-network choice.
It is still too easy for insurance companies to deny claims and make life difficult at best for someone who needs specific care or medication.
And the definition of affordable often strains the definition.
Unfortunately this bill was the best that our corrupt, dysfunctional Congress could write and pass. It is nowhere near what most of us would like to have been the result.
Perhaps Obama, if he had been a more experienced arm twister, could have gotten a better bill written. We are damn lucky we got what we did and to lay the blame on Obama is just an understandably emotional rant.
Sure throw Obama and the rest of the Dems under the bus. You think it can't get worse? Sure it can.
Our 'representative' government sucks. Most people are uninformed. Politicians just throw shit on the wall and whatever sticks they go with. Who here thinks the Republicans will enhance the ACA vs. gutting it? They're busy throwing a lot of shit and if enough sticks then we can get back to the good old pre-ACA days.
And you won't be able to kick Obama around anymore.
grahamhgreen
(15,741 posts)I take it you've looked into getting the drugs overseas... India. Thailand, etc.
theboss
(10,491 posts)Those are fun.
lostincalifornia
(3,639 posts)President was called
unionguy
(6 posts)I have never voted for anyone with a R next to their name and never will. I agree that the ACA has and will help millions of people. That said , this president has some responsibility for how the ACA has come about. Call me old fashioned but I still believe that a leader leads by example. In my opinion the president should have, on day one, took his hand off the bible, walked over to John Bonehead shook his hand and then kicked him square in the nuts. Then did the same to Mitch the little Bitch. The President is the leader of their party. His example reflects the position and direction that party takes. He had a Dem majority for 2 years. Did he take the lead against Rethug aggression and interference? No he did not. Instead he spent 3 years kissing their asses trying to compromise. You be nice to a Rethug and all you get is mugged for your trouble. He has also spent the whole time kissing Corporate Ass, hence the ACA as it is written. I'm on a medication that costs $10,000.00 a month, no that's not a typo. Thank god and my union that I still have insurance coverage. They are self- insured with a local insurance company administering the plans. I have been eligible for Medicare for 3 years, but because of Part D, I found it cheaper to stay on my Union Retirees insurance, which still costs me over $900.00 a month. An ACA plan that is even close costs $1050.00 a month with higher deductibles. It sure would have been nice if I could get the help of subsidies to off set some of my medical expenses. I now pay almost 50% of my income for medical expense. If I buy an ACA plan I can get 3-$400.00 a month from the government to help, but because I have a plan from my union (which is better and cheaper ) than a ACA plan, I get no help. The President and the Dems screwed us union people big time. The only union people who could get the subsidies, because of income, would be early retired (62) , or disabled & early retired,(as is my case). I'm not very happy with this situation myself. Will, I feel for you, without the support of my union I would be in even worse shape. Keep up the good fight.
Sunlei
(22,651 posts)About 20,000 a year retail in medication costs.
Yet when Doctors without borders gets the same aids medicine to help treat people in other countries, they pay maybe hundred a year total. I think they get their drugs from India.
I wish there was someway we could cut out the 'for profit' middlemen from insurance & medicine sales. They price gouge everyone, including our Federal funds we hand over to them!
Ms. Toad
(36,471 posts)We have several medications which are covered by some companies, and not by others. Whenever we change insurance companies, the first thing we do is check to see if the critical doctors and care facilities are on the new plan. The second is to check the formulary. The third is to check the less critical doctors.
MS medication, medication for IBD (which my daughter has), and often AIDS medications are ones which a fair number of insurance companies have classified as specialty medications (typically biologics). I am surprised it caught you off guard - because it isn't the ACA, it is insurance companies in general. The last 3 insurance plans I have been on have classified my almost off patent, non-biologic, medication as a specialty drug - which means it is covered, but at a % of the cost rather than a flat fee. The current plan (as of January) has it back as a formulary-name brand drug. More expensive than most, but better. She's also on a prescription probiotic - nearly as expensive as your wife's medication. Fortunately, two of the last three have covered it - but the two prior to that didn't.
Appeal. Most insurance companies have an appeal mechanism based on medical need. You will need strong doctor advocates on your side - and you may have to step through (or document that you already have) first/second tier medications to prove they don't work and your wife needs the medication she is on. We've had to do it both ways - repeating trials of medicines or procedures that hadn't worked, and merely documenting that we had already tried it. That run-around is partly because they figure no one will bother and it saves them money - but there is a medically valid reason as well. Doctors are susceptible to marketing - and they may be prescribing medication that is more costly (and sometimes less proven) than other less splashy medicines with big advertising bucks behind it. Having a process of walking through a protocol verifies that the pricier medication is really the best balance of cost v. benefit.
Finally - check to see if the pharmaceutical companies have a compassionate care program. They often offer free or substantially reduced cost prescriptions.
Good luck - and when open enrollment comes around, check the formulary!
bvar22
(39,909 posts)...or over the telephone from The Exchange?
I don't remember an option that let me check "The Formulary".
Of the 5 Million who have bought the new ObamaCare Insurance,
how many do you believe checked the Formulary
or even know what that means?
This is not something we should have to do,
and not something that the majority of Americans are equipped to do.
REP
(21,691 posts)It has nothing to do with the ACA or the website. You can obtain a formulary from the website of the insurer or call and request one.
Things I check for in insurance: formulary, DME, labs and imaging, surgery and hospitalization co-pays.
bvar22
(39,909 posts)...through the Healthcare.gov website or over the phone,
HOW many of them do YOU believe "checked the formulary",
or even KNOW what that means?
If YOU and a small handful of others have learned that this is important,
GOOD FOR YOU!!!!!!!
...but what about the MILLIONS who don't have the benefit of YOUR experience or ability?
People who live in civilized countries do NOT have to do this.
ObamaCare was something that was supposed to be GOOD for those who have been unable to afford insurance,
not "throwing them into a Shark Tank with a Pork Chop tied around their necks." (thanks, Will)
We couldn't get through our State's Website, so we had to sign up over the phone.
My Wife and I are educated, intelligent, informed, professional Americans.
Until yesterday, I had no idea what a "formulary" was,
or that I should "check it",
and the option to do so was NOT offered by ANY of the avenues we tried in our effort to get covered.
I will again give you this challenge:
or even KNOW what that means.
Ms. Toad
(36,471 posts)The contact information for any plan sold through the exchanges is easy to find. If I had a condition that required costly medicines, I would have spent considerable time comparing my options - as I did for the last set of plans I had to choose between in the same time frame (October, then again in January). Although the mechanism for signing on the dotted line is different, the process of choosing between plans is identical.
It sucks to be chronically ill.
But anyone with a chronic, costly, illness, has to become equipped to deal with the medical system - whatever the structure. From care through payment. It is a matter of survival. My daughter has been chronically ill since she was 4 (she's nearly 24 now), and my spouse has less serious, but still chronic, illnesses. I would not dream of buying insurance without making sure their drugs and critical doctors were covered, or without estimating what the annual out of pocket spend would be. Medicare - which everyone touts as the model for single payer - has similar challenges and options for drug coverage - well covered in the news for anyone who has not been sleeping for the past decade (at least). I shouldn't have had to diagnose my daughter's most recent chronic illness - but I did. That sucks too. I shouldn't have had to find a drug trial when no approved medical treatments were available. She shouldn't have to be battling her way back from a mental health hell hole her psychiatrist left her in.
But that is the reality of living with a chronic illness - you have to deal with things no one else has to deal with. And unless Will Pitt's wife was diagnosed after they purchased health insurance, it was medical and financial suicide not to take that obligation seriously. And the reality of formularies, or the failure to verify what meds are covered, has nothing to do with the ACA
And if you aren't equipped to sort it out, there are navigators to help you out.
Zorra
(27,670 posts)on edit: And the process of choosing plans is not identical by any stretch of the imagination.. My healthcare.gov website page never worked. I had to do everything over the phone. Because every individual is offered different plans according to state and circumstances, I had certain plans available to me. All I had to go on in choosing a plan was the healthcare.gov supervisor, telling me the basic benefits of the plans available to me. It took 2 1/2 hours on the phone for me to choose a plan. This was after 63 days of determined, persistent work on my part to finally get to the point where I finally had a possibility of being successful.
Blah blah blah, and I actually have some of the conversations with healthcare.gov recorded. It's too bad I didn't get it all, it would probably be worth a fortune as a comedy skit
No offense, but no one except someone who did not experience the intense, illogical, nonsensical prolonged core stupidity of the fubar healthcare.gov system can understand how "Call the company!"is a roflmao, "let them eat cake" moment for those of us who ran the gauntlet and survived with our reason still somewhat intact.
I kid you not, many of my conversations on the phone with healthcare.gov were more ludicrous than this monte python skit below. I'm serious.
Ms. Toad
(36,471 posts)post ACA than it was before. Speaking as someone with a child whose medical bills are $60,000 a year - in a good year. As much as I would love to wave my magic wand and make everything better, it ain't gonna happen.
People with chronic health conditions have more challenges than those who don't - for a whole host of reasons. Nothing that anyone can do will change that. And people with chronic health conditions have to protect themselves because people and systems created by people are imperfect - and no one else is in a position to protect them, or will. Even with the best of intentions, and good training, my daughter's doctors are going to be two steps behind her, and a step behind me in assessing what changes in how her body mean she may have acquired one of the dozen or so cancers she is at risk for. No matter how perfectly the insurance companies perform in claims processing, people (and computers programmed by people) make mistakes. Even if we get a Medicare like system, there will still be mistakes - my father has been battling over a coverage dispute for months. And, no matter which system we have, no one is going to spoon feed you that cake. And when the cake doesn't make it to your mouth, and you have a chronic illness, it hurts more.
You can give up and let things happen to you (and then get mad when not even cake makes it to your mouth), or you can be proactive and utilize what is available to the greatest extent possible.
I've been living with this reality daily for two decades - "them" is me. And I'm thrilled to finally at least have more nourishing cake - and a bit cranky at people who don't take simple steps to protect themselves (like checking formularies - which anyone with a chronic illness who has had health insurance should be well acquainted with) and then blast the cake - because blowing it to smithereens only serves those who want things to go back to what they were. Which sucked a whole lot more.
Zorra
(27,670 posts)I'm simply telling the truth. As for myself, I prevailed, against all odds.
For many people, like me, negotiating the program was a seriously fucked up nightmare, to put it nicely. And I am far more educated, in more ways than just academia, than the general population of the US.
"Calling the company", before I was a verified cash cow for them, was a fruitless enterprise.
You want to know why so many people who seriously need insurance are not signing up for the ACA?
It's because they have no clue, on this formerly green earth, what a formulary is. Nada. Or why they should ask about formualries, and other such pharmaspeak blah blah blah.
The process, especially in red states like mine, has been scary and/or seemingly impossible for far too many people. I know, I sign up poor folks for Medicaid, or ACA plans income dictating, at every opportunity.
I'm not trying to blow the ACA to smithereens, I'm only recounting my experiences, in order that someone who should fix it will fix it.
Denying that something is kind of a mess won't fix the mess.
And the bottom line here is, the real mess originates with for profit health insurance corporations.
We need a simple public health care system, like Canada has.
I have many friends from Canada. I make it a point to ask them, "How do you like your healthcare system?"...
The common answer is "what's not to like, eh?
It's free."
Ms. Toad
(36,471 posts)by someone who has the intellectual resources to negotiate the system, and every reason to know what a formulary is (unless his wife was just diagnosed), who has a following, and who certainly seems to be trying to blow it to smithereens.
That is different from acknowledging that it is imperfect. And as much as we need a public health care system, it would never have passed in the first place and - if by some miracle it did pass, the challenges to implementing it would have made the living on the edge of terror that I have been doing waiting for 2014 and praying that the law was not gutted before them seem like a mere speed bump.
And - as far as calling the company before I was a verified cash cow - I have had to do that with nearly every insurance policy I have had for the last 15 years (at least a half dozen policies). Never once has one refused to answer questions about the formulary, or the doctors, I would have access to. And I do it because I know that my daughter's life depends on having access to specific medications and, to a lesser extent, the doctors who have been treating her for years. And when I have issues with coverage, I work the system. I don't go into a public forum, with full knowledge of the weight my name carries, and call the person who put his political reputation on the line to obtain this significant step forward a "piece of shit used-car salesman" and start a second nearly identical thread when I've said something so offensive that I'm locked out of this one.
Zorra
(27,670 posts)health insurance companies. That's really tragic; hopefully, the ACA will be the doorway through which we can eliminate this working the system nonsense forever. My ACA subsidized plan is excellent, relatively speaking. But my premiums after subsidy generally cost between 6% and 8% of my net monthly income. My net monthly income is variable month to month. A reasonable value, that I feel fortunate to be able to afford without significant hardship.
I am pleased that folks are sharing their experiences in public forums, as a way to generate discussion, raise awareness, and elicit ideas for possible solutions to the problems of having to work the system in order to insure that they or their loved ones would get adequate health care.
I suspect most of those who have been frustrated by the system empathize with emotional rants, they know how authentic they are, most having probably at some point smashed a small household item or two when frustrated by dealing with the bureaucracies related to the for profit health care industry
With all due respect, I believe you may possibly be jaded by this long experience in learning to be an expert at dealing with insurance companies. If I was to go around and ask ten of my neighbors what a formulary is, nine of them would probably have absolutely no clue. A major problem with the ACA, IMO, seems to be the official assumption that everyone understands the rules and the ins and outs of working the health insurance system, that everyone has good reading comprehension skills, and that everyone has knowledge of how to use a computer, and how to negotiate cyberspace effectively. This is a mistake, these things frighten people who are ignorant about them, and these are formidable obstacles which they avoid because it all seems like rocket science to them.
Effectively, it really is rocket science for them.
You are very fortunate to have been so well accommodated over the phone by these companies it has been my experience that many people do not always have that kind of experience. In fact, when I am conversing with intake staff in the offices of health care providers, I often mention the problems I have had with health insurance companies. I have seen many of them roll their eyes, and tell me that they know the drill and could tell me stories.
I talk to people about insurance and the ACA in my daily life. I carry the phone number of the local ACA navigator at all times. I call the navigator and set up appointments for people on the spot. I give out the healthcare.gov number to people who potentially have the wherewithal to negotiate the system over the phone, barring programmatic requirements or system failure. I helped my closest neighbor sign up for Medicaid. I helped the disabled man who works on my guitars sign up for Medicaid. I helped co-workers and friends get signed up for much needed semi-affordable health insurance coverage.
The reason I do this is because I understand that they are afraid. Some have been propagandized by the RW, others are afraid of looking stupid, or afraid of failure. They don't know what to do, and I do know what to, so I do it for them, without much personal time expended. If I asked all the folks I have assisted what a formulary is, 90% of them wouldn't the slightest clue.
I know for a fact that it is a huge mistake to assume that people understand the ins and outs of working the health insurance, system, because most really don't.
http://www.democraticunderground.com/?com=view_post&forum=1002&pid=4696750
krawhitham
(4,967 posts)This was for Ohio
Zorra
(27,670 posts)it is convenient? Even if it is just a link for Ohio, it might be a key to finding them in my state.
I help people sign up for the ACA, and if I could find the way to access the formularies for different companies and their plans, it would be very helpful.
Thanks!
chompers
(22 posts)Puke. A few years back, the OP would have been crucified for the FBHO bit. I fully agree.
pansypoo53219
(22,083 posts)complain about it. to congresscritter or media.
Catherina
(35,568 posts)Your wife is lucky to have you be her side and fighting for her. I hope this nightmare ends soon so you don't have this added, cruel burden to deal with and can peacefully devote your time to her instead. I'm so sorry.
Whisp
(24,096 posts)oh, I know..... !
[URL= .html][IMG]
.html][IMG] [/IMG][/URL]
[/IMG][/URL]
Cha
(309,260 posts)turns out can just be misguided.
gulliver
(13,364 posts)I'm embarrassed for you. Yeesh.
LittleBlue
(10,362 posts)My mother had MS before she passed.
I hope your wife gets the medicine she needs. It's a fucking crime the way this system is run.
truedelphi
(32,324 posts)And it is especially galling to think that these pathetic situations of people finally getting "insurance coverage" but then having to be wiped out economically in order to get drugs, that this is all occurring after the system was supposedly "reformed."
tritsofme
(19,036 posts)I hope you take your own advice, and attempt the anatomically impossible, within the next 24 business hours.
jazzimov
(1,456 posts)finds and takes advantage of a loophole in the ACA, and you automatically say FU to the President for trying to do the right thing?
I agree with the FU to the insurance industry. BUT you lost me when you said FU to the one guy who fought with blood and tears trying to do the right thing for all of us.
Response to jazzimov (Reply #668)
Post removed
Riftaxe
(2,693 posts)are off limit to ACA plans.
Actually why should we do that? The fucking huge increase in deductible is fucking untenable, fortunately Senator Reid solved that by calling us all liars...
You want me to vote what again in 2014?
Some of the younger people will wonder why they can't be an asshole all the time, and watch gains turn into loses...this is why.
You know well why i hate you WilliamPitt, but on this travesty I do believe we can be united.
MineralMan
(148,792 posts)If not, why not self-delete this. I know you can't post in the thread, but I believe you can still self-delete it. That would be a good thing, I believe, and it could drop out of sight and not embarrass you any further.
Logical
(22,457 posts)MineralMan
(148,792 posts)at all. Did you miss that part of the OP?
questionseverything
(10,654 posts)without addressing cost containments was a mistake so it all has something to do with potus
you wrote a good op addressing the high cost of drugs and listing some possible solutions, can't we build from that and let potus know it needs fixed instead of going back to this denial thing?
Response to WilliamPitt (Original post)
Name removed Message auto-removed
Cirque du So-What
(27,992 posts)nobody will remember that you wasted a few minutes to register for this site - much less your aptly-chosen username. Dunces are a dime-a-dozen, yunno.
itsrobert
(14,157 posts)n/t
crimeariver1225
(19 posts)donheld
(21,320 posts)People don't have to believe he is that, but people, even at DU, should have a right to say it.
Whisp
(24,096 posts)riversedge
(74,817 posts)Hit the spot with your post. While it is good to vent the anger--the IP will help the opposition also.
Babel_17
(5,400 posts)I can't say I wouldn't say the same thing if I was in a similar situation. The POTUS is going to be getting blessed, and cursed, a lot as the ACA gets implemented. Max Baucus should be sharing in that but he wasn't that public a figure.
It's a credit to the DU that we don't censor, what is painful to hear, because it is expedient.
The pain and suffering here is something we need to take into account.
BoulderNative
(1 post)William Pitt. Who are you? Are you one of us?
I am from Boulder and I am the fearless leader of all the people there.
